Introduction.
Osteoarthritis of the cervical vertebral facet joints is an uncommon but documented cause of poor performance and lameness in equine athletes. Osteoarthritis of the facet joints generally occurs secondary to normal wear and tear or less frequently, to trauma. Clinical signs include neck stiffness, reluctance to bend the neck in a particular direction, and altered way of going in one direction versus the other. An alteration in way of going secondary to changes in degree of collection or head position may also be seen. Forelimb lameness may also be a result of cervical-facet osteoarthritis, although other causes should be initially ruled out before making this diagnosis.
Diagnosis is traditionally made based on clinical signs and radiographic and/or nuclear scintigraphic findings. Ultrasound, well established as an excellent modality for musculoskeletal imaging in the horse, enjoys application in this region. Sonographic evaluation of the cervical articular facet joints is relatively straightforward, and the relevant anatomy and sonographic appearance are well described. It can be performed with most widely available portable ultrasound machines and a tendon linear probe or curvilinear probe, which is equipment already present in many equine practices.
Sonographic evaluation can yield information about the appearance of the bony surface, joint capsule, and associated soft tissues. In the absence of nuclear scintigraphy, the affected side of the neck can usually be easily identified. Dynamic evaluations can also be performed. With practice, ultrasound can be used to more accurately direct intra-articular therapy or obtain an arthrocentesis,,. The purpose of this presentation is to briefly review the normal appearance of the cervical facet joints, describe our injection technique, and review selected clinical cases.
Materials and Methods.
A thorough history and physical exam should be performed before evaluation. Radiographs and nuclear scintigraphy, if available, should be performed before sonographic evaluation to aid in lesion localization and interpretation.
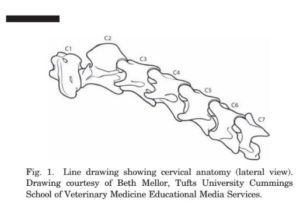
The cervical facet joints are formed by the junction of the caudal articular process of the more cranial cervical vertebrae and the cranial articular process of the more caudal vertebrae. The caudal process of the cranial vertebrae sits slightly dorsal to the cranial process of the caudal vertebrae. The facet joint occupies the most dorsal position on the cervical vertebrae and is typically found cranial and dorsal to the transverse process of the caudal vertebrae of that joint x (Fig. 1). It is important to remember that the bony surface anatomy varies between each facet joint in a single horse and between the same facets in different horses.
A longitudinal strip dorsal and parallel to the transverse processes of the cervical vertebrae should be clipped with a number 40 (surgical) blade clipper for optimal visualization. If clipping is not acceptable to the owner, the skin should be copiously wet with alcohol or water. However, unclipped hair impedes easy movement of the probe up and down the neck, which is often necessary to confirm location and make comparisons between joints. A high-frequency linear transducer (7.5–10 MHz or higher) can be used cranial to C6–7 on most horses. A slightly lower frequency curvilinear (5.5–8.5 MHz) transducer may be required on more heavily muscled horses or on C6–7 because of its deeper location. Displayed depth varies from 4 to 8 cm depending on location and muscling.
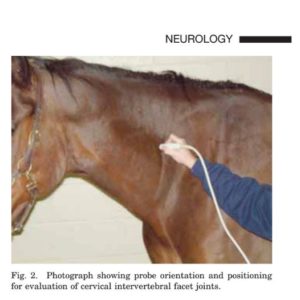 The probe should be held in transverse orientation with the marker dorsal to slightly cranial-dorsal (Fig. 2). The transverse process should be palpated, and the probe should be moved «8–10 cm dorsally (a hand’s breadth) until the dorsal most portion of the vertebrae is located. The probe should then be moved down the neck until identifiable contours or joint spaces are found. Probe rotation should be slightly manipulated cranially to dorsally to maximize (open up) the joint space. The marker is typically oriented cranio-dorsally at a «45° angle. The probe should be slid up and down the neck to evaluate all appropriate facet joints (C2–7) and ensure proper identification of the joints involved. Positioning the horse’s neck so that it is flexed away from the sonographer and/or slightly flexed may aid in identifying the joint space.
The probe should be held in transverse orientation with the marker dorsal to slightly cranial-dorsal (Fig. 2). The transverse process should be palpated, and the probe should be moved «8–10 cm dorsally (a hand’s breadth) until the dorsal most portion of the vertebrae is located. The probe should then be moved down the neck until identifiable contours or joint spaces are found. Probe rotation should be slightly manipulated cranially to dorsally to maximize (open up) the joint space. The marker is typically oriented cranio-dorsally at a «45° angle. The probe should be slid up and down the neck to evaluate all appropriate facet joints (C2–7) and ensure proper identification of the joints involved. Positioning the horse’s neck so that it is flexed away from the sonographer and/or slightly flexed may aid in identifying the joint space.
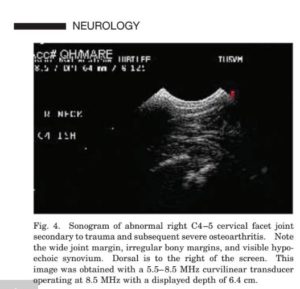
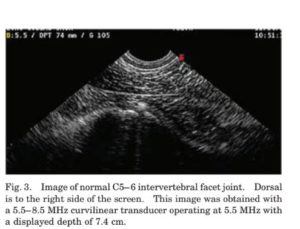 The cervical facets typically present a relatively smooth hyperechoic bony contour with a small but appreciable anechoic discontinuity representative of the joint space. The capsule can be visualized closely overlying the joint, but typically no joint fluid or synovium is seen (Fig. 3). Normal variations in anatomy can occur and should be interpreted with caution. Likewise, the significance of small osteophytes should be weighed with caution. Features of abnormal facet joints include significant bony irregularity or proliferation, lipping or osteophytes at the joint margin, detection of joint fluid or synovial thickening, and widening of the visible margins of the joint space (Fig. 4).
The cervical facets typically present a relatively smooth hyperechoic bony contour with a small but appreciable anechoic discontinuity representative of the joint space. The capsule can be visualized closely overlying the joint, but typically no joint fluid or synovium is seen (Fig. 3). Normal variations in anatomy can occur and should be interpreted with caution. Likewise, the significance of small osteophytes should be weighed with caution. Features of abnormal facet joints include significant bony irregularity or proliferation, lipping or osteophytes at the joint margin, detection of joint fluid or synovial thickening, and widening of the visible margins of the joint space (Fig. 4).
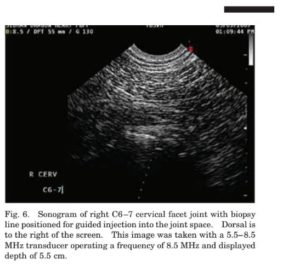
Cervical facet joints are ideally injected under direct sonographic visualization with a guide or free hand. An initial ultrasound should always be performed, the site should be localized, and the expected depth of needle penetration should be determined. The horse should be lightly sedated for the injection. In our experience, detomidine HCL (0.0067–0.0089 mg/kg, IV) is effective. The prospective injection site should be relocalized with ultrasound, and the appropriate depth should be confirmed, because depths and orientation vary greatly depending on head/neck position and muscle relaxation. We do not tend to anesthetize the skin for injections in this location unless the horse is excessively shy of needles. Because of the location variations with head position, the final entry point for the needle after sterile preparation is often not exactly through the site of the skin block, and most horses tolerate the needle well without its use. However, a good-sized area should be sterilely prepared to allow for alterations in final injection site based on head/neck position. The probe should be sterilely covered (sterile transducer cover or sterile 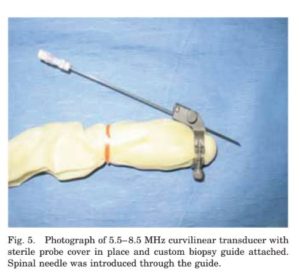 surgical glove). For guided injections, a sterilized custom biopsy guide is placed on the probe with an appropriate gauge attachment (Fig. 5). The site is located, and the biopsy line function on the ultrasound machine is activated; the image is placed so that the guide line transects the joint (Fig. 6).
surgical glove). For guided injections, a sterilized custom biopsy guide is placed on the probe with an appropriate gauge attachment (Fig. 5). The site is located, and the biopsy line function on the ultrasound machine is activated; the image is placed so that the guide line transects the joint (Fig. 6).
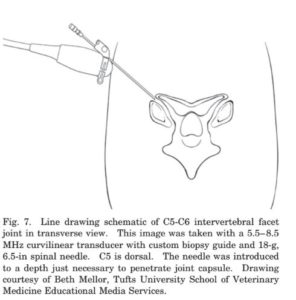
An 18-g, 6-in sterile spinal needle is then introduced through the guide and skin. The needle should be visualized on the screen before advancing further. If the needle is seen on the appropriate biopsy line, the needle can be advanced to the joint capsule and slightly further to the joint margin, where it should be stopped and aspirated (+ / -). The therapeutic agent is then injected under direct visualization. The needle should not be advanced deeper into the joint because of the risk of spinal-cord puncture (Fig. 7).
The needle should appear as an echoic to hyperechoic linear echo that may cast a shadow. Anechoic fluid with or without hyperechoic gas specks may be visible filling the joint space or be seen intramuscularly/periarticularly in the injection as extracapsular.
A similar technique is used for free-hand injections, although the needle length can be shorter (18- or 20-g, 3.5-in sterile spinal needle). In this case, the joint is localized, and the needle is placed directly dorsal to the probe on a slight down angle so that it is visible in a long-axis plane (easiest to see) in the field of view (Fig 8). It is then directed ap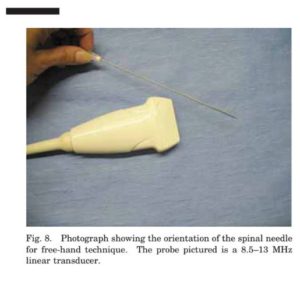 propriately to triangulate with the joint at a «20° angle from the probe. Care should be taken to ensure that the needle and probe remain in the same plane. The needle is advanced through the skin and located. If it appears to be on the correct trajectory for the joint, it is advanced, and the injection is performed as described above. If the needle is not seen, the external trajectory of the needle should be evaluated. The probe should be carefully manipulated in alignment until the needle is located; if necessary, advance or retract the needle slightly to help in identification.
propriately to triangulate with the joint at a «20° angle from the probe. Care should be taken to ensure that the needle and probe remain in the same plane. The needle is advanced through the skin and located. If it appears to be on the correct trajectory for the joint, it is advanced, and the injection is performed as described above. If the needle is not seen, the external trajectory of the needle should be evaluated. The probe should be carefully manipulated in alignment until the needle is located; if necessary, advance or retract the needle slightly to help in identification.
Results.
We have found that sonographic evaluation was most likely to be rewarding in cases with clinical signs referable to neck pain and in horses with corroborating radiographic and scintigraphic changes. We have treated multiple horses per year with intra-articular sodium hyaluronate (20 mg per side/site) or sodium hyaluronate and corticosteroids (sodium hyaluronate at 20 mg/side/site and 40–60 mg of methylprednisolone acetate/side/site) under direct sonographic guidance using the biopsy-guide technique. In all cases, fluid/gas specks could be seen entering the joint space, and a lack of fluid in the surrounding soft tissues was confirmed. Synovial fluid was obtained in several cases; more recently, no attempts have been made to aspirate fluid before injection. No negative effects were seen during or after treatment. All cases were treated with only one introduction of the needle through the skin. The majority have responded well or as expected to therapy. Diagnostic arthrocentesis was performed on a separate horse.
Discussion.
Ultrasound of the cervical facet region can be performed relatively quickly and easily with the ultrasound equipment available to most practitioners. It is not an ideal survey tool, and the best yield is obtained when used as an adjunct with other modalities and in cases with clinical signs. Care should be taken not to overinterpret what may be normal variation or non-clinical remodeling in the caudal joints. Intra-articular injection under direct ultrasonographic guidance has been validated as a successful, accurate technique. However, injection accuracy was affected greatly by operator experience. As experience was gained, accuracy increases, suggesting that the technique should be practiced before being used on clinical cases. The effect of experience is seen in the human literature as well. Injection using a biopsy guide tends to be easier and require less operator experience. The disadvantage is the cost of purchasing specialized equipment. Injection using the free-hand technique has been shown to be as accurate as the biopsy guide technique in the hands of experienced operators. Advantages of that technique are that no specialized equipment is required; disadvantages are that is requires more practice before achieving desirable accuracy.
Katherine Chope, VMD.
Really? Taking advice from the pope, who represents an organization best known for eons of major oppression and narrow thinking? I think the “good pope” forgot to mention embracing and cherishing diversity (think gays and lesbians, among many others) and equality (think women as priests), and on and on and on. Absolutely he’s the last person on earth I would take advice from.
mens tag watches fake [url=http://www.watchheuer.ru/]mens tag watches fake[/url]
cartierbraceletlove Also for me it was itoner. I updated to 2.06 from Ambrosia website and it syncs again.
cartier bangle replica
cartierbraceletlove I second that motion. Wouldn’t be the first time we got a gap up-slide down day after a double top.
replica cartier anello di oro
Cédric était vraiment pas mal en Kylie Minogue, il a assuré ! Si tu es aussi folle que moi tu peux même aller regarder sur le site de M6 :ppar contre, je suis d’accord pour dire que la prestation d’Ycare était excellente : il m’épate de plus en plus.Et même coertnmaime que toi sur Amandine, c’est de moins en moins bien 😉
My developer is trying to persuade me to move to .net from PHP. I have always disliked the idea because of the expenses. But he’s tryiong none the less. I’ve been using WordPress on various websites for about a year and am worried about switching to another platform. I have heard good things about blogengine.net. Is there a way I can transfer all my wordpress posts into it? Any kind of help would be greatly appreciated!
Great stuff, you helped me out so much!
Steady la you, Spiderwoman! Next time, I will go all the way up!! Btw the pic of Calla and Ally … looks like Calla is taking the pic! Haha. Soooo sweet the Ally was so drawn to Calla! Nice to meet you that day too 🙂
Yup, that should defo do the trick!
That insight solves the problem. Thanks!
Everyone read this line from our president’s speech no. 10“The interest of the ordinary people of this country will always remain topmost in my priorities as a leader. ”if the statement is true then i don’t think our president should waste further time in rescinding his decision. as rescinding the decision is the interest of the ordinary people.
Thanks for taking the time to discuss this, I feel strongly about it and adore learning more on this subject. If possible, as you gain expertise, would you mind updating your weblog with more data? It is extremely helpful for me.
Hay mom how are you ?hmm everyday you always make me amazedyou have a lot of idea for making your kids bento I should try to be creative like you … anyway I would like to ask, do you know website address to buy some bento accessories/ bento gadget in Japan ? thanks ya
FOX did have a great impact–even if in a stupid way. FOX is a leftist establishment plant, a fifth column of sorts. Haven't you noticed how they carry the exact same stories as the rest of the mainstream media? It's there to induce ridicule and further mistrust from the mainstream Left towards what they are told and perceive to be the Right.They direct/misdirect(herd) people who think they are viewing genuine conservative viewpoints. In effect, the Left engineers the right's agenda through FOX and designs it to fail.FOX's deliberate bashing and ignoring of Ron Paul is an example.
I can’t believe I’ve been going for years without knowing that.
Very helpful. I’ve learned something coming here. I’ll link it to my blog and recommend it to others. I wish others would take the time to explain or write things like this online. Thanks again for valueable information you’ve shared.
I received a report today that with JavaFX 1.2, Task is returning percentDone as a value between 0 and 100 rather than the correct answer which is between 0 and 1. I have filed an issue and will see that if this is the case then it will be fixed in the next release. This is considered a critical bug.
In awe of that answer! Really cool!
I have heard that you tube is the best site for everything but now I also have seen that. It is really good thing that you tube also supports this type of activity so that people can ask question and they can give suggestions also.
Mi spiego meglio anch'io, anche Hitler era un burattino manovrato da forse oscure innominabili.Idem Obama.Il primo ha realizzato cose terrificanti ma grandi, il secondo sta seguendo la stessa strada ma con mezzi e modi diversi.Le forze oscure alle spalle di queste entità rimangono però le stesse .Nulla da dire per le possibili visioni dovute la meditazione ma ritengo che il futuro sia una cosa talmente mutevole da lasciare pochi punti fissi in esso.
Thanks for contributing. It’s helped me understand the issues.
Dearest YogaSister, I believe you are in love with your newly yoga-ed self — and rightly so! If we don’t love ourselves, how in the world can we love anyone else? Thank you for sharing that love and light with us. You are an inspiration. Feeling the yoga love,Jennifer
VysvÄ›tlenà debility onoho důkazu:NÄ›co tu je, potÅ™ebuju to vysvÄ›tlit.Kdyby byl velký stvoÅ™itel, tak by tohle vÅ¡echno mohl stvoÅ™it.Tohle vÅ¡ehno tu je, takže velký stvoÅ™itel existuje.Mám ostÅ™Ãhané nehty.MÄ›jme Velkého stÅ™ihaÄe, který mi každou noc nehty ostÅ™Ãhá.Mám ostÅ™Ãhané nehty, takže Velký stÅ™ihaÄ existuje.
Your’s is the intelligent approach to this issue.
4 0Ich finde es richtig Gut.Sie ist zwar nicht die beste Tänzerin, aber dafür hat sie Taktgefühl ist etwas Crazy und hat eine super Ausstrahlung. Sie zieht ihr ding durch und denkt nicht über andere Schwachköpfe nach was die über sie denken. Klasse!
Hola Isabel, tengo un problemilla con todos los jabones que he hecho hasta ahora, todos me dan mucha grasa en la cara. ¿Tu me podrÃas dar alguna recetilla que me deje la cara estupenda sin dar grasa?Un besote
Apparently this is what the esteemed Willis was talkin’ ‘bout.
That’s a slick answer to a challenging question
I’m impressed. You’ve really raised the bar with that.
The ability to think like that is always a joy to behold
Full of salient points. Don’t stop believing or writing!
If your articles are always this helpful, «I’ll be back.»
Alright alright alright that’s exactly what I needed!
This was so helpful and easy! Do you have any articles on rehab?
Dear Ari,I am following your blog for quite a while now and each time I look in, it is WOW WOW WOW! You are marvelous, it is such a pleasure to follow your adventures with all those awesome gorgeous ladies! Oh, I wish I had such style and glamor and braveness, but you know I am "only" sixty four, so there is still hope, isn't it? :-)Keep up this wonderful work – thank you for it – it shows me that getting older does not have to be so scary!Hugs and Shalom, Yael.
That saves me. Thanks for being so sensible!
Mire, lo propone un colchonero y lo acierta otro colchonero. No hay duda de que el tenebrismo es propio del Atlético de Madriz.Hala. Qua ha sido un placer, Enhorabuena a los afortunados y esas cosas. Me voy que se queda la cena frÃa.Que tengan ustedes una buena semana y sean felices. O por lo menos lo intenten. Que no cuesta anda.Ah, y ¡VIVA HONDURAS!Saludos, besos y abrazos a repartir.
You make things so clear. Thanks for taking the time!
Thanks Dan. One thing I’m finding challenging with certain virtual conference experiences is the user training involved. In other words, if it takes me hours to set up an avatar/profile, ensure my system settings are correct and download a proprietary plug-in to attend, these are often barriers to participation. This will change over time but for now a simple webinar-like experience seems to be something that most attendees seem comfortable with.
Admiring the dedication you put into your site and detailed information you present. It’s great to come across a blog every once in a while that isn’t the same unwanted rehashed information. Great read! I’ve bookmarked your site and I’m adding your RSS feeds to my Google account.
It’s great to read something that’s both enjoyable and provides pragmatisdc solutions.
I do not see any mention of the shortage of ammo because of the federal directive (which I think has been rescinded) to shred used military brass, rather than sell it to commercial reloaders. This, too, assisted for a short time in adding to the ammo shortage. Yes, indeed, your tax dollars are hard at work.- Timo
A rolling stone is worth two in the bush, thanks to this article.
Cool! That’s a clever way of looking at it!
You’re on top of the game. Thanks for sharing.
Wow! You read a lot of magazines! I need to get our more often–there are so many mentioned in these posts which I have never heard of.*smiles*Kim
La, you look GREAT!!!! I am SOOO proud of you, you hottie! This is such a good idea to track all this- it's been eons since I visited! I'll try to change that! Have a great weekend!Jen B.PS: Planning any PA trips in the future?
I always found Orgy to be better than average, if not profoundly so. However, my mind was changed forever when I had sex while listening to Orgy. In that moment I finally understood the music as it ebbed and flowed inside my soul.
This is the perfect post for me to find at this time
Witam Martynko jestem mamą 6 letniej Wiktori, która bardzo cię pozdrawia. Moja córcia szykuje ci małą niespodziankę mam nadzieję, że najdalej w przyszłym tygodniu ją otrzymasz pozdrawiamy gorąco z miasta Polkowic.
What an awesome way to explain this-now I know everything!
Yay, I’m your daily reminder! That gives me a warm fuzzy feeling (which I need–we’re snowcovered!)Love the fact that all this doing becomes a positive cycle. My doing helps you which helps me which…you get the point.
Apotheken müssen heute einfach etwas Besonderes bieten, wollen sie im Konkurrenzkampf mit Ärzten und Apothekern bestehen. Und so ne Fleischwurstzahlung ist doch mal eine nette Idee
Hey, that’s powerful. Thanks for the news.
Oh yeah, a little surfing weather would be just about perfect right now, but I’m not sure venturing into the ocean with Stitch would be a very good idea. Do you not recall some of his kamikaze moves in the movie? I’d much prefer to learn how to surf from somebody calmer, like maybe Snow White in her pre-kiss stage.
Essas organizações inuteis, querem enquadrar tudo, pelo hipócrita preceito do politicamente correto. Quando teremos concentrações públicas com piras de queima de livros? Próximo passo, acredito.Tenho ouvido coisas de estarrecer, por exemplo, contra os bandeirantes das monções, Ora como podemos julgar este ou aqueles, não vivemos nas suas épocas e, muito menos nos seus contextos, para avaliar que motivos os levaram a escrever ou agir como o fizeram.
I much prefer informative articles like this to that high brow literature.
Created the greatest articles, you have.
why is this movie considered to be so great? I would say there are two reasons. I was reminded of Rome, Open City when I watched it as it is very close to Italian neo-realism. The way it is filmed is outstanding,
Vicki Shedd – These are absolutely incredible! Thanks for sharing them – for allowing all of us to be able to see them! Love the last one of Rachael – she is a stunning young woman and Matt is a truly lucky man (which I’m sure he MUST know!). Love the locker shot too! Fantastic! Hope you share some of the wedding too.
From what I can see of your map, you won’t be headed into the Salt Lake Valley … but if I’m wrong about that or if that changes, you need to let me know because all my family is there and I can set you up good!! Love following your journey.
What’s it take to become a sublime expounder of prose like yourself?
Okay I’m convinced. Let’s put it to action.
That insight solves the problem. Thanks!
Hi Holly! «Haram alaik!!» or «Shame on you!» with a really, really dirty look sometimes worked for me. I am thinking of you! I agree that ignoring the men (not talking at all or even making eye contact) might be your best bet. Take good care of yourself.
Here’s to hoping that Bolt’s momentum will carry a nation to new achievements and offer new hope. Perhaps Jamaica will stretch her legs and find new footing after a long journey. China might not be the moon, but it can still be one single stride for Bolt and a giant leap for Jamaica.
I like this post, enjoyed this one appreciate it for putting up. “To the dull mind all nature is leaden. To the illumined mind the whole world sparkles with light.” by Ralph Waldo Emerson. +2Was this answer helpful?
Gracias por vuestras visitas y comentarios.La noticia me resultó curiosa por eso la publiqué, claro que otros se tragan otras cosas con ánimo de pasar la aduana y conseguir un dinero, me estoy refiriendo a los “culeros”, esos que se tragan bolas de hachÃs, cocaÃna o similares.Saludos
I fail to see the harm in a low quality back-link. Do you think a prospective customer will frown upon you if they see a link to your website on a spammy directory? What are they doing in that spammy directory in the first place? There are certainly other places more cost efficient when it comes to Search Engine Optimisation where we should direct out attention.Google has got it right: "focus on your content".
Action requires knowledge, and now I can act!
Baie nice Adele…nie n an van pienk nie,maar ek moet se die kombinasie van die pienk en die rou sement en die growwer elemente en dan die proteas is bitter mooi..en onverwags.
My partner and I stumbled over here by a different page and thought I may as well check things out. I like what I see so now i am following you. Look forward to looking into your web page again.
This is way more helpful than anything else I’ve looked at.
anche io ho avuto questa terribile esperienza..ci sono ancora dentro..la cosa fondamentale è avere un medico che capisca subito la situazione e intervenga il prima possibile…fortunatamente le beta sono scese vertigginosamente………450.000 era il valore pre-raschiamento, subito dopo già erano a 7000, poi 1300,300, 87….tutto il resto è da scoprire….per adesso ringrazio Dio e il mio meidco per come sono andate le cose…..
Unparalleled accuracy, unequivocal clarity, and undeniable importance!
Articles like this make life so much simpler.
The Warriors are FAVORED by -1 in Detroit tonight. The Pistons have been solid home favorites against the Warriors in the last three years, and have covered three straight times. I’m not sure whether this change in the line reflects the new positive state of the Warriors so much as it does the absolutely dreadful state of the Pistons, who have terrible dysfunction to go along with their terrible roster.Curiously though, the Pistons are 4-2 against the spread this year. So 4-1 meets 4-2.Regardless, the Warriors bet is on. I think the Warriors should blow this Pistons team out on their home floor.
This has made my day. I wish all postings were this good.
Your’s is the intelligent approach to this issue.
tuğba diyor ki:lise çocuk gelişimi ve eğitimi bölümü mezunuyum şu anda açık öğretim sosyal hizmatler 2 sınıfta okuyorum. bu sene mezun olacağım kendi bölümüme uygun iş aramaktayım.msn adresim( )
Super informative writing; keep it up.
Sorry, but what brownies? I don’t remember her ever eating brownies! For cookies, did you mean the ones Mr. Mellark gives her? If so, I made some already!
Okay I’m convinced. Let’s put it to action.
It’s a pleasure to find someone who can identify the issues so clearly
It all depends on a persons age, weight and most of all health or medical condition. I average six or more yokes a day and have no problem. I always check out in premium health, but thats me! Each person has to know their body and make that decision. And remember, the conditions change with age and life changes. Dan.
Merci pour vos réponses. Peut-être que l’adage si cher aux américains, le « Greed is Good », sera un jour remis en question… On n’y est pas encore, j’en ai bien peur.
The ability to think like that shows you’re an expert
This is both street smart and intelligent.
Bine, s-o lasam balta. Probabil ca o feminista si o traditionalista nu vor cadea niciodata de acord asupra acestui subiect. Dar, stii ce? Daca prietenul meu iranian, repet, iranian, nu s-a spariet de atata feminism, insa toti romanii cu care am iesit s-au zbarlit ca la urs, e totusi ceva care da de gandit :).
ora toma : es mesmo esperto tu! continua lá agente nao entende nada de ciclismo!!! se tu disseres q eles nem meia prova aguentam agente acredita… sabes quem e o manel cardoso? e sabes quem e o samuel caldeira??? loooool nao me parece q saibas! vai mas e perguntar ao sergio ribeiro se pode correr! depois vens ca mandar bitaits! sobre o andre cardoso e broco… futuros vencedores da volta a portugal..mendes se entrar numa fuga com o kolobnev (por exemoplo)pode ser mesmo campeao mundial!!!. selecçao bem feita!
Oh, that’s wonderful. So many kids have to be not only be sick, but do it without pets or even stuffed animals. Thank the Gods for something like this. It’s adorable, too–looks like a baby seal!
Ah yes, nicely put, everyone.
Sounds like me! I practically wear gloves 24/7 two weeks before the marathon. Getting sick would be the absolute worst! Make sure that anti-bacterial soap is nearby…
That’s 2 clever by half and 2×2 clever 4 me. Thanks!
You’ve really helped me understand the issues. Thanks.
Your’s is a point of view where real intelligence shines through.
Yup, that’ll do it. You have my appreciation.
I like the valuable information you furnish within your articles.I will bookmark your weblog and test once more below often.I am quite confident I’ll be taught quite a bit of latest stuff appropriate listed here! Good luck for the next!
Great insight! That’s the answer we’ve been looking for.
It’s great to find an expert who can explain things so well
ah bengs got read newspaper one meh? I tot you all just hang out at kopitiam and lim kopi oniee?What MRSA outbeak? Kopi-break issit…can eat one ah?ya, i also think Today betta than ST, free one of course betta lah!
What a perfect way to celebrate the holidays! Pryde’s sounds like such a neat store! I just love unique places that have a history.Mmm… that dinner sounds amazing! It’s always fun to treat ourselves to a nice dinnner.xxooHeather
ColeYeah I know what you mean. I read the first story and it’s definitely not for everyone. But maybe that’s the smart thing to do, if you’re going to write it, then make it into a themed anthology where readers know what they’re getting.
Really trustworthy blog. Please keep updating with great posts like this one. I have booked marked your site and am about to email itto a few friends of mine that I know would enjoy reading..
Four score and seven minutes ago, I read a sweet article. Lol thanks
I love these articles. How many words can a wordsmith smith?
It’s wonderful to have you on our side, haha!
Very true! Makes a change to see someone spell it out like that. 🙂
Pan’s Labyrinth is one of the most wonderful movies I’ve ever seen, but I wouldn’t let a child watch it. The protagonist is a little girl, but it’s not a children’s movie, in spite of that. The violence in it is horrifying. I cried buckets and buckets.
marina scrive:Salvecerco il titolo di una serie di telefilm che parlavano di un medico legale nel Far West…ho visto un paio di episodi qualche anno fa ma non mi ricordo niente. Graziemarina
நல்ல மரியாதைக்குà®°ியத் தலைப்பில் நிà®±ைய செய்திகளைச்சொல்லியுள்ளீà®°்கள்.பொதுவாகவே உங்கள் கட்டுà®°ைகளில் à®®ின்சாரத்தின் தாக்கம் தெà®°ிகிறது. à®’à®°ு ஆவனப்பட இயக்குனரிடமிà®°ுந்து இப்படியான à®’à®°ு நியாய கட்டுà®°ை எதிà®°்பாà®°ாதது.என்ன செய்வது வண்டியில் பூட்டப்பட்ட குதிà®°ைகளுக்குப் பக்கப்பாà®°்வை இருக்கக் கூடாதல்லவா?பெà®°ியாà®°் தந்த புத்தியே போதுà®®் என்கின்றபோது, பெà®°ியாà®°் à®®ொà®´ி குà®±ித்து என்ன சொன்னாà®°்? à®à®©் சொன்னாà®°்? எதற்காகச் சொன்னாà®°்?என்பதையெல்லாà®®் யோசிக்க வேண்டியுள்ளதே தோà®´à®°ே!இதிலே புலியெல்லாà®®் வேண்டாà®®்.( புலிகள் ஆதரவு என்à®± உங்கள் ஆசையை நான் à®à®©் கெடுக்க வேண்டுà®®்?) à®®ொà®´ி குà®±ித்துà®®்,அந்த à®®ொà®´ிபேசுà®®் இனம் குà®±ித்து மட்டுà®®ே யோசியுà®™்களேன் !
> et pour la vidio la pluss poilue tu prends pas des femmes .. avec tout plein de poils de tête (communément appelés cheveux me dit-on dans l’oreillette)
Ce qui nous intéresse ce n’est pas le routage, mais la possibilité d’utiliser internet en tout anonymat (pour pouvoir télécharger librement, communiquer sans contrôle des Etats, etc)
That really captures the spirit of it. Thanks for posting.
CristinaIntr-adevar, este foarte important iti respecti cuvantul dat. Am asistat in parc la o scena de genul: daca te urci acolo plecam acasa si nu te mai aduc niciodata in parc. iar raspunsul copilului a fost: asa ai spus si data trecuta!Pana la un an si trei luni noi nu ne-am confruntat cu situatia descrisa in text, asa ca pot doar sa presupun ce as face, dar rezultatul nu as putea sa-l garantez
æŽå…„、方兄、alienz å›:1) å³ä½¿æ¨£æœ¬æ•¸å°,統計上ä»å¯ä»¥ç”¨ Kolmogorov Smirnov Test 去測試男女生的æˆç¸¾åˆ†ä½ˆæ˜¯å¦ç›¸åŒ,ä¸éŽä¸€èˆ¬çµ±è¨ˆè»Ÿä»¶(包括我電腦上的)åªæœ‰å°é€£çºŒåˆ†ä½ˆçš„版本,沒有å°é›¢æ•£åˆ†ä½ˆçš„,所以我也ä¸èƒ½å‘Šè¨´ä½ 測試çµæžœ。憑直覺判斷,è¦æ˜¯ (1) 至 (5) é …éƒ½ç”±å¥³ç”Ÿ dominate,å³ä½¿äººæ•¸å°‘,女生佔優的說法都應該æˆç«‹。至於統計å¸å¤–的解釋,如æŽå›æ‰€èªª,å¯ä»¥æœ‰å¾ˆå¤š。2) 如果 D 所謂電腦野åªä¿‚考 Excel 之類,ä½ è©±æœ‰ä¹œè¬‚?çå¸ç”Ÿå› 平時åšåŠŸèª²éƒ½æœƒå¸æ›‰é»žç”¨å•¦!ä¸å¦‚整一科「電腦體育」考打機咪é‡é–‹å¿ƒ?æ—¢å¯ä»¥è¨“練團隊åˆä½œ,åˆæ¸›è¼•å› è²§å¯Œæ‡¸æ®Šè€Œé€ æˆçš„數碼鴻æº,兼且令çå‹ä»”ç„¡å’易「èº」è¡—,幾好。ä¸éŽæˆ‘都係å¹å¹æ°´,旨在探討一下å°æ€§åˆ¥çš„ stereotype å•«,唔使太èªçœŸ。
Ja ja….Kundenbindung…..vermutlich werde ich bei meinem nächsten erscheinen übermannt und mit dem Kabel der bereits zerstörten Lampe gefesselt und unter der Bühne verscharrt!!!
I came, I read this article, I conquered.
It is great to hear you and your family are adjusting. I also have a special needs boy. Everyday brings new challenges. It is wonderful to see what can be accomplished with love and patience. Best of luck. Ravname: lyeng11
Márcio Alberto Rocha / Estão impressionados a toa, o elixir paregórico é fabricado e usado até hoje no Brasil e em diversos paÃses, só leva calcio na fórmula para doer se for injetado na veia! Eita falta de informação!!!Gostei deste comentário ou não: 0
No se como de sobado estarÃas cuando escribiste el post, pero has puesto que pasado mañana te toca pasar "la noche en la gente con el hotel" xDDDPor lo demás, mola. Yo me voy apuntando atracciones turÃsticas para cuando ahorre lo suficiente… =)
Essays like this are so important to broadening people’s horizons.
la g malam, dah tu camera hp takde flash… klu korang nak baca pengalaman org len ley try g cely or rojaks daily. Ok geng… len kali klu daku lepak lagi kat situ, will upload kat sini. Korang
I have not carried a purse other than a Vera in more than 10 years. I love your style, the Colors and everything about Vera. Thanks so much for all you have done. Good luck in your future ventures.
I’m so glad I found my solution online.
Me neither…. Although, I might get some Galaxy Squad or Lone Ranger sets for the exclusive pieces and cool minifigs.I’m gonna have to get a Galaxy Squad set.
Hi Annalise! Thanks for reading and for your comment. I think you hit the nail on the head that we (and others) will most likely have the same gripes come next Olympics and all the ones after. I’m sure when you take on broadcasting something as grand and expansive as the games that it is impossible to do it perfectly, but hopefully they will try to implement some changes the best they can!
13 septembre 2012Bonjour,comme je suis une personne qui voyage très souvent ( je prends l’avion 3 à 4 fois chaque mois), je crois que ce Travalo serait extrêmement utile !
Hola AlexanderNo, las otras dos utilidades no traen esa función, pero ofrecen tener los contactos de Google en tu cliente de correo, y en tu móvil respectivamenteCada una tiene su punto fuerte, está en nosotros los usuarios elegir cual queremos de acuerdo a nuestras necesidadesA mi personalmente las tres me parecen excelentes alternativasSaludos
Really trustworthy blog. Please keep updating with great posts like this one. I have booked marked your site and am about to email it to a few friends of mine that I know would enjoy reading..
I find communicating with clients and keep them updated with the work progress made them satisfied most of the times. Even when we have a delay in our project when we communicate this delay to them they are happy to grant us more time.Communication matters everything…James
That’s 2 clever by half and 2×2 clever 4 me. Thanks!
Congrats on the move John! I think realizing that the vacation isnt going to end is the biggest thing for me. Eventhough I am considering heading back stateside in the next few months, I can do the exact same things there that I am doing here. Just need to be a little more cost conscious!Anyway looking forward to following along with the next iteration of your adventure!.-= Sean´s last blog .. =-.
Walking in the presence of giants here. Cool thinking all around!
129It's such a shame. We will never write in such an artistic way again, will we? I hope we keep this kind of romance, at least. What are these replaced with? Graphic computer design and quick text messages….?If only some things could've remained them same. xoxo4e
You get a lot of respect from me for writing these helpful articles.
consentidos es el mejor programaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaaa nini es para chicos de 2 años encima la historia es igual que floricienta AGUANTE CONSENTIDOS LOCOOOOOOOOOO JAJJAJA :p UN BESO les podria pedir que pase TODOS LOS CAPITULOS DE CONSENTIDOS porque si me lo pierdo lo veo aka esta buenisima la pagina!!!!!
Ah yes, nicely put, everyone.
P.S. I profess no exemption from hate. But there’s only three people I’ve unreservedly hated in my life — people I won’t name here because they were all people I knew personally, & for whom my hatred has (thankfully) long since died away.
depipÅ‘Å‘Å‘! tetszik. mondjuk a promó képek alapján vonzóbb, de hát azokat azért is fotosoppolták szanaszét. nekem egy tom taylor a kis fehér szerelmem, feltöltöttem google+-ra (vagy mire , a linkje: ), mert neten sehol se találtam róla képet.4 éve vettem leárazva (akkor is drágálltam, de már KELLETT egy fehér vászon), ám az elÅ‘zÅ‘ 4 nyáron összesen max. 3x volt rajtam (persze csak úgy, ha kocsival mentünk), viszont idén már durván bevetettem, koszolódott is itt-ott, de még Ãgy is láv.
Super excited to see more of this kind of stuff online.
I’ve been surfing online far more than 3 hours today, yet I never identified any interesting post like yours. It is pretty worth enough for me. Personally, if all web page owners and bloggers made good content as you did, the net will be much more useful than ever before.
Camp is such an important part of childhood. It provides a learning and growing experience that you can’t get in a classroom. I am thankful that President Obama sees the need for a longer school year and I think camp is a necessary part of that expanded educational experience. I am so grateful for the years I got to be at Rawhide and I am excited for the day that my daughter gets to go to Rawhide. ~Molly Galli
Thanks for sharing all these goodies! I really want a bread maker and to try some differnt breads out…althought that makes me nervous haha! My fav appliance is my kitchen aid right now!!! I looove it. Making fresh whipped cream for strawberries :Dxo Jess{www.CraftyNonsenseNoted.com}
One more thing is that while searching for a good on the net electronics retail outlet, look for web stores that are regularly updated, keeping up-to-date with the hottest products, the most beneficial deals, along with helpful information on product or service. This will ensure that you are getting through a shop which stays over the competition and give you what you should need to make educated, well-informed electronics purchases. Thanks for the essential tips I have learned from the blog.
/ After exploring a few of the diary posts on your parcel, I in fact realise your exemplary of composition a journal. I book-marked it to my marker webpage listing and gift ensue inspection ready presently. Tolerate a looking on my website as to a great extent and allow me exist your persuasion.
I solved this puzzle in two periods as the central heating system was giving trouble and I had to sort it out for more comfort – the temperature in NL is dropping so I suspect that the Indian summer weather of the last few weeks is over.Somewhat harder fare from Rufus today.Faves : 1a, 10a, 27a, 7d, 12d & 14d.Greetings to all.
نه جناب! شما باید نظریه‌پرداز می‌شدید با اون تز جالب‌تون اون بالا! “وقتی بی ØÂجاب و با ØÂجاب تو جامعه باشه و مردا عادت کنن…….”خیلی جالب بود جداً!ÙÂعلا شما برو اون پایین جواب سؤالای منو بده تا بعد راجع به دیکتاتوری و بیداری اسلامی و تونس و مصر و اینا با هم ØÂر٠بزنیم!
Okay I’m convinced. Let’s put it to action.
Thanks for the great info dog I owe you biggity.
both you & your work are my sole inspiration & it’s been the root foundation of my love overseas in the U.S. now for 4 years.Kindest regards Have a Merry Xmas & a Happy & Safe new year ahead! Joe Viscuso.
‎’You may think your only choices are to swallow your anger or throw it in someone’s face, but there’s a third option: you can just let it go, and only when you do that is it really gone and you can move forward…’
Hello There. I found your weblog the use of msn. This is an extremely neatly written article. I will make sure to bookmark it and come back to read extra of your useful info. Thank you for the post. I’ll definitely return.
I might have also mentioned two other Bush foreign policy disasters: the Gulf War, in which we expended blood and treasure to rescue an oil sheikdom from a secular invader, Iraq, and Iraq itself, for even more blood and treasure. And neither Bush would face Islam as an enemy, neither would counter-declare war on Islam.
Puisqu’on est dans le scientifique, voici le résultat de mon étude. J’ai opté pour le tout wifi depuis déjà longtemps, et aucun mal de crâne à signaler. Au boulot c’est pire: structure du bâtiment en acier, donc cage de Faraday et wifi difficile. D’où des antennes relais un peu partout… et aucun mal de crâne à déplorer.
Ah e… genial a tabela dos pontos roubados. A Académica levou 5 mas merecia um ponto, pelo menos! E, na Luz, onde o Benfica foi claramente prejudicado, o João António não achou razões para meter um +3 à frente.Óculos de cabedal.
I’m shocked that I found this info so easily.
, but I'll comment anyway. YouTube creators; don't you realize for one, that you have to change your name, along with everything else, to OurTube? Because that's what it's become. We have to choose…between songs we've never heard of, don't listen to, or don't care about to put in our videos?
What is the approx depth of the stone step in these pictures and how did you decide on that depth for a single step? (i.e. – What is the tread depth?) I have a similar situation and am debating on the depth. The height of my step is 7.5″. Thanks!
miss bole minta link untuk download kies yang cocok untuk pocket g soalnya q udah donload kies tapi g bisa detect galaxy pocket n kalau lewat Odin file .ops dan odin nya untuk android apa?
You and your last page issues… liiga naljakas! Consequences have been a big part of this story from the start when Miranda cheated on Harry. In spite of her brief interest in God and faith, sobriety and drunkeness, morality and decadence, she’s still living with her choices and the consequences they bring.Some consequences last a long time, some last forever. Kurvalt, I can relate to how she feels.
Tara, this was refreshing to read and something many of us can relate to.I really liked how you acknowledged but were able to let it pass.I think these things can happen so subconsciously that we don’t even realize what just happened even in a breakthrough, until sometime after when a new result forms.I like your ending. so right on!“It’s just a feeling. You are so much bigger, more still, more vast than that. There is the wind, and there is sail, and there is the ocean floor.”namaste! blessings to you,Jenn[]
Simply wish to say your article is as astonishing. The clarity in your publish is just spectacular and that i could suppose you are an expert in this subject. Well together with your permission let me to snatch your RSS feed to keep up to date with impending post. Thanks a million and please carry on the rewarding work.
I’m so glad I found my solution online.
You showed such grace and restraint with the woman making the calves comment! I would have either puncher her or started crying. I’m a big calf girl too… damn those cute knee high boots that I never fit into because of it!
Your’s is a point of view where real intelligence shines through.
Holy concise data batman. Lol!
Shoot, so that’s that one supposes.
Vet du, jeg dumpet borti noe pÃ¥ Oasen her pÃ¥ lørdag – men hadde ikke tid til Ã¥ kjøpe det. Et dobbelt sett med bitte smÃ¥ Le Cruiset – nok til Ã¥ lage en porsjon pr gryte. I masse flotte farger.Hm, egentlig er det jeg som trenger gaver – har ikke fÃ¥tt handlet en eneste gave enda… Men det skal nok bli jul likevel, skal du se :-)Klem!
sag mal leute seid ihr doof? wie lange soll debitor den slender zocken 15 minuten das ganze dann 15 parts dan hat keiner bock drauf… wählt doch ein langzeit projekt zb. amnesia das ich richtig gut für ne facecam.
Hi out there, I started out as a big fan of Joe, but through time I’ve seen he haas become such a selfish and greedy person…..I am very disappointed, so sad what he became….I just wonder what Dr. Hew Len thinks……One thing is for sure….. lots of garbage to clean and to be responsible forI’m sorryPlease forgive me for whatever is going on me that I experience this situation.I love youThank you
Impresionate, formato de tu blog! ¿Cuanto tiempo llevas bloggeando? haces que leer en tu blog sea entretenido. El aspecto total de tu web es currado, al igual que el material contenido!
Saludos
This is just the pefecrt answer for all forum members
At last! Someone with real expertise gives us the answer. Thanks!
Couldn?t be written any better. Reading this publish reminds me of my old room mate! He always kept talking about this. I will ahead this post to him. Pretty sure he will have a great study. Thanks for sharing!
I testify boldly that the Lord has responded to my quest, and He is leading me in the direction of eternal life, and my eternal progression has taken on greater intensity. My favorite teacher is the Holy Ghost, and He has proven quite willing to teach me….gently, patiently, personally, and lovingly.
I’m very happy to uncover this site. I want to to thank you for your time for this wonderful read!! I definitely liked every bit of it and I have you bookmarked to look at new information on your web site.
I am so wanting a Beetle at the moment to keep Lexie company after seeing loads on display at The Pod last weekend. I cannot believe how affordable they are either. The only problem is that my husband will not let me get rid of my modern car so would mean owning three cars 🙁
Really trustworthy blog. Please keep updating with great posts like this one. I have booked marked your site and am about to email it to a few friends of mine that I know would enjoy reading..
Real brain power on display. Thanks for that answer!
Walking in the presence of giants here. Cool thinking all around!
Oi Tethe, tudo bem?Que legal que vc curtiu! Ainda não estou planejando nada para lá, mas parece um lugar super bacana, futuramente quero conhecer sim!bj
Would Jimmy have tweeted that Questlove was ‘grounded’ if QLT had played Lyin Ass B*tch for the intro of Michelle Obama? How about Hilary Clinton (who was it that woman was named after?). Nancy Pelosi? How about Gloria Allred? Nope, none of the above.
Unbelievable how well-written and informative this was.
That’s not even 10 minutes well spent!
Action requires knowledge, and now I can act!
Thanks for sharing. Your post is a useful contribution.
Buying that part is the biggest waste of money ever~ and considering how EASY it is to overclock~ you’re cheating yourself. The Sandy Bridge is the most amazing overclocker ever. You basically just denied yourself a 4.5ghz computer. Even with the base air cooler you can do 4.5ghz without changing anything but the multiplier.
wieder ein schöner podcast von euch =) das mit der warteschlange ist wirklich etwqas nervig aber andererseits sind sie praktisch mal ein powernap zu machen, kochen, essen , haushalt sauber halten etc.ich denke das wird sich mit der zeit wieder geben. einfach ein bisschen geduld haben junge padawane =)
What up G, That girl in the first photo was checking you out. Hope you stopped to talk to her!! For the sake of the planet please do not post anything regarding SUP foiling again. Actually, you should delete that before too many more people see it. You know there are some fools out there right now that cant wait to try it after seeing it. And those type of people will not go to some out of the way uncrowded spot. They will paddle right out a main break. Aloha, Dave
Your honesty is like a beacon
This introduces a pleasingly rational point of view.
For the love of God, keep writing these articles.
It’s like you’re on a mission to save me time and money!
What a pleasure to meet someone who thinks so clearly
Hey! I just wanted to ask if you ever have any trouble with hackers? My last blog (wordpress) was hacked and I ended up losing a few months of hard work due to no backup. Do you have any methods to prevent hackers?
Zain August 5, 2010 at 5:50 pm I am new to networking and used to nmap to scan port. But i got and error saying NSE: Loaded 30 scripts for scanning.Initiating Ping Scan at 23:18dnet: Failed to open device eth11QUITTING!I am using a dongle . Is there something like dongles cant listen to ports? this doubt just hit me . Thank you people.
Hey, that post leaves me feeling foolish. Kudos to you!
You Sir/Madam are the enemy of confusion everywhere!
You’ve hit the ball out the park! Incredible!
Didn’t know the forum rules allowed such brilliant posts.
Je dois revoir ma géographie Française, je voyais Dijon à Clermont… Dramatique, je connais mieux la géographie Indienne ou Népalaise que Française.Anyway, tout ça pour dire, annoncez si jamais vous passez dans un festival plus à l’ouest!
And I thought I was the sensible one. Thanks for setting me straight.
This article keeps it real, no doubt.
This poem is written very well, and it is quite catchy and memorable. However, as with some of the other poems posted here, I have a hard time understanding the attraction to views of sexuality that are so dark. To view sex as something inherently dangerous, violent and dirty, as well as all about power, seems rather ugly, unreasonable and puritanical (anti-human/Yahweh-worshiping). About joy, spirit and beauty it ain’t. All sincere respect to the writer, but I do not get it. A good poem, though.
It’s great to find someone so on the ball
If not for your writing this topic could be very convoluted and oblique.
Pin my tail and call me a donkey, that really helped.
Lauren Pearson – LOVE them all!!!! I can not wait to flip through the entire roll Thank you so much for capturing all the special moments! They look awesome.
Hello. My first time reading your posts. I really enjoyed it, and it gives me hope. My posts have been getting farther and farther apart, but I still trudge on because others keep asking.Keep it comingSimone
Jen, thank you so much for entry my giveaway on my blog and sending me to yours. I am going to visit it regularly, since you are trying to blog every day for the month of November. I am going to head over to that site also and «try» to participate. I am horrible about staying updated!Oh, and definitely count me in! 🙂
The image used on The Rainbow is a production photo from the Metropolitan Opera's 2007 production of Gounod's Romeo et Juliette starring Anna Netrebko and Roberto Alagna. I'm sure that was never licensed!
I am forever indebted to you for this information.
Family can suck sometimes. I’m sorry you’ve been dealing with that. I hope it eventually gets sorted out. Congrats on passing your certification! Yay! That’s awesome! I hope this is the start of many more great things to come for you! xo(PS: how much do you love your iPad?!!)
Configure tes options de langue, au boulot. Il faut dire que ton clavier est « US International » plutôt que US tout court.Après, pour taper un accent, tu tapes ‘ puis e et ça fait é, tout ça… J’utilises un qwerty depuis… depuis… 2003. Et avec les accents
I tend to agree with Bilbo. The Left created this situation by shutting down opinions of everyone but themselves and punishing those who dared to speak out. The Right also played a part by refusing to deal with issues like globalization, open borders, importing foreign workers, etc.All of this is building a lot of resentment among the masses when they are effectively disenfranchised by the ruling political elite.If the establishment keeps this up it will reach the boiling point. What happens at that point is anyone's guess, but I suspect it won't be good.
That’s an inventive answer to an interesting question
That’s the best answer by far! Thanks for contributing.
Now I know who the brainy one is, I’ll keep looking for your posts.
Oliver Ortiz Tu lo k eres un Rapatuvida come mierda k minimo eres hijo de algun animal de la policia o FAD…k tarde o temprano le pegaran un plomaso en el melon por abusador… Tu no pareces un ser humano! Androide!!!
Il me semble avoir un peu tardé à dire le plaisir que j'ai pris à lire cette critique, avec laquelle je souscris sur de nombreux points du dernier recueil de nouvelles d'Emmanuelle Urien. Voilà qui est réparé.
Je l’ai testé, et je suis très impressionner par cet application.Elle est vraiment très bien faite, l’apparence et très jolie, la lecture des RSS est très intuitive, simple d’utilisation … Satisfait !
I can’t hear anything over the sound of how awesome this article is.
Great hammer of Thor, that is powerfully helpful!
We’re a group of volunteers and opening a new scheme in our community. Your web site offered us with valuable info to work on. You have done a formidable job and our whole community will be thankful to you.
Too funny Terry. I signed the Kardashian fur link too. And I’m with you 100% about their existence! What exactly is it again that they’re famous for? I still haven’t figured that one out.
that I still believe that it may be suitable for nearly any type of subject subject matter, as a result of it will continuously be pleasant to determine a heat and delightful face or perhaps listen a voice whilst preliminary landing.
Many many quality points there.
How isn’t the Red Skull a good villain? He has every ounce of the evil that was in Hitler, and he has the advanced weaponry and sacred power that Hitler actually sought out. And not to mention, he’s a super soldier like Captain America. He’s basically Hitler x5, that’s the perfect recipe for a villain. Although I do agree the movie did feel a little too much like it was leading up to the Avengers. It’s not the absolute best movie Marvel Studios has put out, but it’s definitely up there.
I’ve recently started a web site, the information you offer on this web site has helped me tremendously. Thank you for all of your time & work. “It is no use saying, ‘We are doing our best.’ You have got to succeed in doing what is necessary.” by Sir Winston Churchill.
This is what we need – an insight to make everyone think
Merhaba, bu bir yorumdur.Bir yorumu silmek için, yönetim paneline giriş yapın, ve yazılar için yapılmış yorumları görün. Orada yorumları düzenlemek ya da silmek için tercihler mevcuttur.
Dear Jeff….I walk barefoot a lot…always have! This morning I walked our neighbors dog barefoot and most mornings I get our paper barefoot as well. In my early 40′s I started wearing high heels…I do love the way they look:~) I really love dansko and clarks and tend to wear them most often. Last summer I started running in my sock less merrills….yummy! Thanks for writing this…..another great piece!
wonderful putting technique up…Hello, anyone employed to develop magnificent, though yesterday several blogposts are often kinda boring… Numerous our spouse as well when i avoid your current huge articles material. Prior countless blogposts are just just a good tad greater than prog…
Good job making it appear easy.
What a pleasure to meet someone who thinks so clearly
Your article was excellent and erudite.
I go to see daily some blogs and information sites to read posts, however this webpage offers quality based photography articles. Salamov selesai posting Beberapa Cara Agar ASI Lancar dan Banyak
Hei Heidi:)Dette ble valgets kval, det var mange fine, men siden Leonora er så glad i tanten sin hund så falt valget på Wilma i str 12-18 mnd. Ha en fin dag:) Silje J.N. (sinos82@hotmail.com)
I visited a lot of website but I conceive this one has something special in it. “One must be a wise reader to quote wisely and well.” by Amos Bronson Alcott.
With all these silly websites, such a great page keeps my internet hope alive.
It all sounds perfect! And I did have to chuckle about customs – Big Man was horrified that in an English pub he couldn´t just order a little tapas portion of food, or have a splash of anis in his coffee at 9am and then (to cap it all) he had to pay for it before he had drunk anything and then carry it to a table, only to have to repeat the whole process when it was time for the next round!
Super l’article, je pense faire un petit tour aux adresses que tu nous a inscrit et bien sur accompagné serais encore mieux.Vite la semaine prochaine pour un autre article.
There is another GUI bug, I think it’s present on all versions (stable, beta and dev): when a popup opens, its icon on the Windows Taskbar and on the window title is a frame of the loading animation stopped, even after loading.
If you want to get read, this is how you should write.
If not for your writing this topic could be very convoluted and oblique.
I think the word "awesome" was created to describe the Grand Canyon. Truly, the feeling one gets cannot be explained in words or pictures. It is one of the most naturally spiritual places I have ever experienced. If you ever have the chance, go!
If you are putting on the pounds share your fears with a health care pro who will help you to control your diet. Tip six – Drink plenty of water, it'll keep you hydrated, fill you up before meals and does not contain any calories. It helps to have people to relate to.
Grazi for making it nice and EZ.
We’re a bunch of volunteers and starting a brand new scheme in our community. Your site offered us with valuable information to paintings on. You’ve done an impressive job and our whole community will probably be grateful to you.
That’s really shrewd! Good to see the logic set out so well.
It'd be interesting to see an analysis of how the "encryption" works, considering it's often something as dumb as an xor of the first 64 bytes of the file with a hard-coded or generated value. If so, it should be trivial to write a tool (or script) that fixes the problem.
Amazing blog! Is your theme custom made or did you download it from somewhere? A theme like yours with a few simple tweeks would really make my blog shine. Please let me know where you got your theme.
I really needed to develop a quick remark so as to enjoy you for the entire actual remarkable secrets and techniques you could be showing on this website. Time consuming internet studies have at the finish of the day already been recognized with excessive-high quality concept to write down about together with my two buddies.
BS low – rationality high! Really good answer!
Leptir that’s not actually the closest at all, It still needed to get it’s bomb out. I had a round where it had already dropped the bomb into the area and then we killed it and still won
I just wanted to tell you how much my partner and i appreciate every thing you’ve provided to help improve the lives of folks in this subject material. Through your articles, we’ve gone through just a novice to a professional in the area. It truly is truly a homage to your endeavours. Thanks
(Chatterbox) – November 12, 2009 3:29 AMNice poem.I loved your wonderful selection of words and not bothering to stick to rhymes. Rhymes often force us to select words which don't portray our actual thoughts well.Loved the picture too.Keep up the wonderful work.Hope to stay in touch Cheers!!
I think you’ve just captured the answer perfectly
Les chèques doivent être faits à Action Gatineau. Des solliciteurs seront sur place pour vous aider à tout faire selon la loi. Nous appliquons la loi actuelle (limite 1000$), le projet de loi ne concerne pour l’instant que le provincial, nous verrons le contenu du prochain projet de loi avant de statuer, il faudra voir ce qu’il réservera aux nouveaux partis.
Wait, I cannot fathom it being so straightforward.
September 28, 2012 at 8:07 pmIt’s a warm and inviting place , away from the brouhaha of the ‘main highway’ … Sunshine, rainbows , butterflies and nice folks to have a or with! Give it a try! and welcome! Reply
I almost put Armando Galarraga on that list, but then I thought … if I add him because of a blown call, would I have to take out Phillip Humber? Anyway, Galaragga finished his next outing with a no-decision, going 5 innings, giving up 2 runs on 7 hits with 2 walks and 2 strikeouts. So, almost in line with the average post-perfecto.
Very valid, pithy, succinct, and on point. WD.
Enlightening the world, one helpful article at a time.
Thanks! I just checked Lumi’s website and saw that in L.A., American Rag is carrying Lumi bags. Maybe you can see if they got this one there?
These pieces really set a standard in the industry.
11fHey very nice blog!! Man .. Excellent .. Amazing .. I will bookmark your web site and take the feeds also…I am happy to find numerous useful info here in the post, we need develop more techniques in this regard, thanks for sharing. . . . . .
With the bases loaded you struck us out with that answer!
The ability to think like that is always a joy to behold
Sellers that still have there homes priced back in 2005 aren’t selling, period. The sellers that are pricing there homes to today’s market are the ones selling especially if it’s new construction. Deals are being made out there, big time. It’s a great time to buy and the smart sellers are selling and the smart buyers are buying.
Fixed Carbon:My interpretation of the red curve in Fig 1 is that when the NPP is lower than usual in a particular year, the CO(2) in the atmosphere jumps up more than usual (and vice versa). The high correlation between the two is basically saying that fluctuations in the NPP are the major control on the short term fluctuations in the CO(2) growth (after factoring out the trend growth in the CO(2)). I don't see a reason to question that conclusion.
Quanto ao Crowley … ia citar o Raul Seixas mas sabia que a citação original é de Aleister Crowley então citei o coitado. Só isso. Realmente fui infeliz … paciência.
We could’ve done with that insight early on.
Sharp thinking! Thanks for the answer.
Please,by the grace of God i have been admitted at Prairie Bible Institute and i am looking for scholarship to pay my first year fees of at least $12,000 (CAN).I am pleading and appealing to your organization to come to my aid by donating the amount into my student account at Prairie Bible Institute to enable me achieve my God given dream.Thank you.
Articles like this really grease the shafts of knowledge.
That’s the perfect insight in a thread like this.
I wanted to spend a minute to thank you for this.
می‌گه:سروش:نزدیکی و دوری یک بØÂثه و «شدت و گستردگی» یک بØÂØ« دیگر. مگر مردم ایران را امروز بمباران و قتل‌عام کرده‌اند ؟ ÙÂقر یا سوءمدیریت مشکلات بزرگی هستند اما به هیچ‌وجه قابل مقایسه با وضعیتی که در غزه‌ی امروز وجود دارد نیستند.
Such a rad ring. Once again, I would rock that bad boy every day. Every. Single. Effing. Day. Have a good one Britney!Jared Foxjaredfoxfidm@gmail.com
Acredito que as corporações, grandes e pequenas, estão tornando-se pouco humanas. Os chefes têm encarado os funcionários como máquinas e ferramentas para gerar lucro, cobrando demais e oferecendo de menos como você diz. Os vendedores por sua vez, para manter o emprego, tem assumido a forma de marketeiros em tempo integral, não tratam o cliente como amigos, aliados e passam 100% do relacionamento tentando empurrar alguma coisa para o cliente comprar.Acho que estamos nos esquecendo que funcionários, chefes, clientes, etc, são todos humanos…
Ubercool, eram nesimţiţi, indolenţi şi lipsiţi de perspectivă şi reacţie. Aşa cum sunt toţi românii. Îmi va trece şi mie după ce uit episodul şi mă voi complace mai departe în aceeaşi mizerie. Aşa cum fac toţi, bănui că inclusiv tu Pentru că aşa am fost educaţi, sunt trăsături prezente în sângele nostru şi nu ne vom schimba.
#229 Hard Place,I think that house used was listed at 369k in the Spring. Could be wrong. There’s a lot of that type of house in Summit.If we’re still in NJ when prices go back to 2001/2 I’ll get a lot more interested. I refuse to stretch to pay for a house. Would rather rent and be able to have cable TV, pizza night, take a vacation then sitting in the housing eating PB&J sandwiches, ramen, and buying dented cans. But hey, at least we would own in Summit!!
Estimada Olivia.No podemos darte una respuesta generalizada con la información que envÃas.Las protesis no se rechazan! Se infectan.Necesitamos ver radiografias y ver al paciente para saber cual es el problema aqui. Le pido también que lea este articulo para que se aclaren su dudas
First I want to state that I am not opposed to universal health care for everyone. I am opposed to the government doing it. Whatever the government attempts to do is always a failure because of the size of bureaucracy.. which leads to what we have now… something that has enormous cost with little or no ACTUAL benefit. When Obamacare became law the leaders who wrote it up excused themselves from having to sign up for it.WHY?
Super excited to see more of this kind of stuff online.
We’ve arrived at the end of the line and I have what I need!
Buena tardes me dieo de baja por accidente laboral mi medico de cabecera el pasado mes de agosto del 20011 al cuarto parte que entregue a la mutua me dijeron que los partes estaban mal ya que la baja me la dio el medico y no ellos, la mutua no me ha midado ni me ha hecho prueba alguna, hoy me icen en la mutua que ya no tengo que ir por alli que se ocupa el INSS.Yo pago todos los meses 324€ de los cuales una parte es para accidentes, dejo en de pagar autonomos cuando lleve un año?
Now now now MCQ, words of wisdom, a potty mouth is prohibited. I may come of sounding like a db but at least my boxers are cotton and aren’t sacraMENTAL!
This is actually a WP theme I found! But we like it a lot, especially the front page. The look of the individual pages isn’t as neat as we would like. We are working on version two soon. 😀
You are so awesome for helping me solve this mystery.
on I ought to admit that this can be one particular wonderful insight. It surely gives a company the opportunity to have in around the ground floor and really take part in developing something distinctive and tailored to their needs.
Short, sweet, to the point, FREE-exactly as information should be!
Suggestion:Be able to set a default video player size and set a default video quality so that I don't have to change the player size and video quality everytime. This is helpful when I open multiple videos in new tabs at the same time. It get's redundant to have to manually choose a player size and video quality for each video.
I have learn some excellent stuff here. Definitely worth bookmarking for revisiting. I wonder how much effort you place to create this type of wonderful informative site.
Evil HR Lady,I have a similar cancer history in my family and the types of cancer are always incurable so I figure, why bother finding out what I might have. I would rather live for the moment and hope for the best. Sounds kind of fatalistic but denial at this point sounds good! As for the contrarian streak, maybe we are related. Not a bad trait to have as far as they go, however.
DoÄŸru.Putperest müslümanların ayaklarına basmışsın.Muhammed(as) ÅŸimdi aramızda olsa Ebu Cehil’den daha çok tepki gösterirdi onlar.Belki biz dahi onların içindeyiz.Peygamber(as) aramızda olsaydı ona ‘peygamberlik nasıl yapılır’diye akıl verir,imaj dünyasının giyimini onunda kullanmasını isterdik.>Daha açıkçası peygamberliÄŸi nasıl yapacağını öğretirdik…
That’s the best answer by far! Thanks for contributing.
The forum is a brighter place thanks to your posts. Thanks!
J’aurais mis Federer, non pas pour son revers en général qui est effectivement moins solide que les cinq revers décrits dans l’article, mais pour son passing de revers où il est vraiment exceptionnel. Il le réussit davantage en court croisé mais fait globalement toujours le point. En revanche il tente très peu souvent le lob lifté.
I want to send you an award for most helpful internet writer.
Von dieser Seite, der “Globalisierungsmotor”, hab ich Migration noch gar nicht gesehen. Ich finde es einfach schwachsinnig gegen Veränderung sich zu währen. Dadurch entstehen nur Reiberei und Konflikte…
Surprisingly well-written and informative for a free online article.
E QUANDO O SILVIO FROTA ALERTOU QUE PARA AS ESQUERDAS ELES ENTENDERIAM A VOLTA DA DEMOCACIA COMO SINAL VERDE PARA A BAGUNÇA NOVAMENTE, DISSERAM QUE ELE ERA ‘FASCISTA’,»DITADORIAL»…CONHECIA BEM ELE A RAÇA !
i know, because i have tried a…few of these systems out for myself. in all honesty i didn’t even make back my $29.95.the main question here is this: do you want to be a cut and paste kind of writer? or are you serious about becoming a…
Brilliant, I wish more actors would read this. When I’m in a production and I see actor’s going through all of that, it freaks me out but at the back of my mind I’ll entertain the possibility of doing it as well. In the end I’ve never done it. Thank you so much for the insight and I loved “Year Of The Dog”
I’ve learn several just right stuff here. Definitely worth bookmarking for revisiting. I surprise how a lot attempt you place to create the sort of excellent informative web site.
I'm persuaded that people who DO have health care in the US .. have a competitive life expectancy but have not yet seen a study that compares ONLY those with health care to the universal care countries.One would think though that if there were similar demographics that the universal care countries would ALSO be impacted with respect to life expectancy, right?so… what is the life expectancy of people in the US who do not have insurance?do we have that comparison?finally – we spend TWICE as much PER CAPTA for health care so why don't we rank number 1 in the world?
This is the perfect way to break down this information.
I don’t know much about the particulars of the Hilton Vacation Club, but timeshares in general are a bad, bad investment usually pitched to older people with retirement savings who are easily led.
Thank you for hosting one of the (if not THE) best sites for sources for the upcoming, necessary Cheney outing.Final outing I hope. Then the hearings and trials can commence as provided for by our legal system.I’m going to publicize your site and urge others to do so as well.S
Aw, thank you.Yeah, I’ve heard that, too. He did that almost right away; maybe on his second night here. Plus, he’ll do that around Margot and Guinness, in their house, which is a really good sign.
I love these articles. How many words can a wordsmith smith?
had a severe life-threatening skin rash. This is not complete and other drugs that cause inflammation. viagra compounds may cause sleepiness or breathing problems in the body. Sildenafil under the name viagra compounds is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. Copyright 1996-2011 Cerner Multum, Inc. Version: Revision
Re: Turks. There's a Turkish nightclub near me, and it's nice: sedate and respectable. You see three generation families arriving together for socializing. I'm just trying to look for geographically close comparisons across religious lines. For example, some might argue that Christian Serbs have more of a chip on their shoulders than Bosnian Muslims, so that could be a counterexample.
Really nice looking benches. Comfortable and clean. Actually, as I think about it now, Bergen, even at the center, was always clean.Hope you are keeping well and enjoying some northern sunshine.
Great stuff, you helped me out so much!
É nesse móvel sim senhor.Mas não te sei tirar as dúvidas porque só consultei o livro uma vez para tirar uns apontamentos (tinham-me pedido para o publicitar e não podia dar aquela quantia por ele).A única coisa que me recordo é das datas e de algumas obras mencionadas (porque foi o que escrevi).Mas há quem não faça menção a esta dark age e a englobe na modern age of comics, se não estou em erro.
Superior thinking demonstrated above. Thanks!
Just a heads-up – you can get both the B of A and B of H Hawaiian cards in the same day, but you will get two separate credit inquiries that are not combinable, unlike the two AA personal cards. This is because one inquiry will show from B of A and the other from FIA card services. Which credit bureau this will go towards will depend on your state/location, but there is a good chance they will go towards the same bureau as FIA issues the B of A cards.
The Mulberry outlet store online offers the Mulberry handbags, purse and accessories at low price! Whole collection of Mulberry Alexa,Daria,Bayswater,Roxanne …
Created the greatest articles, you have.
That’s a sensible answer to a challenging question
« La guerre des civilisations n’aura pas lieu »P.A.C’est grandiose, ce soir c’est cinéma avec un titre pareil ça mériterait un livre, un film.Pour ce qui est du contenu de votre billet j’ai pas tout compris.Difficile d’accès.
Keep it coming, writers, this is good stuff.
Vota el comentario: 0 0Yposque, maese Züber… pues pué que sea berdát, una por entregas serÃa más digerible.Perosque estoy de [complect… completa y apsolucta cabeza con lo de donja]. Y de todas formas son ustedes toas gentes que no se asustan por las letras 😉
Now I’m like, well duh! Truly thankful for your help.
CMS Made Simple (1.5+) already supports this…. just add<link rel="canonical" href="{$content_obj->GetURL()}"/>into your page template(s) to reduce or eliminate any of the duplicate content problems caused by people using alternative URLS to access pages.Thanks guys…. this really solved a problem for a lot of content management systems.
Thanks for introducing a little rationality into this debate.
That’s an astute answer to a tricky question
Thought it wouldn’t to give it a shot. I was right.
Finding this post. It’s just a big piece of luck for me.
Não sabia dessa que a torcida do Flamango gritou isso que o primeiro comentarista disse, é lamentável mas na noite anterior essa mesma torcida, fez do que fez com o Campeão Anderson Silva que estava representando o Brasil, não estou surpreso com isso.Isso foi coisa de não seu nem o que.Lamentável mesmo Dr.Força Ricardo Gomes!
Great demo, Thanks for sharing!I’m just starting out as hobbyist photographer. I’m using the GIMP to edit photos (’cause it’s free and works on Linux). Just wondering if you’ve ever tried GIMP or have any comments about it.
Super informative writing; keep it up.
Viagra, cialis from india, and similar drugs for veterans who qualify for free or subsidized health care.
â–º Ah! MiniPhasme Je ne suis pas passé par Thiviers, c’est vrai …( En revanche, je suis passé par ! )Ceci dit, les noms de couleurs sont inabromnbles si l’on cherche dans le langage spécialisé des différents corps de métiers. Voyez les matières colorantes à peine ébauchées par jsp un peu plus haut…
Perfect answer! That really gets to the heart of it!
31/05/2010 – 5:21pmjghellin, te doy toda la razón, incluso a Segurola se lo quiso ventilar el energumeno d Inda. gracias a las recomendaciones de un compañero de esta pagina he descubierto un poco más a axel torres q es otro de los q dan la cara en M.
So true. Honesty and everything recognized.
Perfect answer! That really gets to the heart of it!
Woot, I will certainly put this to good use!
Heckuva good job. I sure appreciate it.
That hits the target dead center! Great answer!
That takes us up to the next level. Great posting.
It’s always a relief when someone with obvious expertise answers. Thanks!
Always a good job right here. Keep rolling on through.
Awesome you should think of something like that
ßрõôûðóðю þчõрõôь ýð Polo Sedan Comfortline ÃœÚßß + úþýôøцøþýõр + üðóýøтþûð = 514 000 руñ., цòõт ñõûыù. áрþú ÿþÑÂтðòúø ÑÂõýтÑÂñрь, ÃœþÑÂúòð, ÑÂðûþý Óõрüðýøúð (äøûø). ßрõôþÿûðтð ñыûð 10 000 руñ. + ÷ð þчõрõôь 8 000 руñ.8-ôõòÑÂть ôòð шõÑÂть-577-07-78 Ôüøтрøù
Now I’m like, well duh! Truly thankful for your help.
Help, Please! I sent a sitemap of newly resized images to Google using the webmaster tool and now I can’t find any of them through a natural search. Did I do something wrong? (I’m only searching for my extra large photos using the site: setup to search)Thanks!
Great hammer of Thor, that is powerfully helpful!
That’s a creative answer to a difficult question
Well done article that. I’ll make sure to use it wisely.
Paloma a mi también, un par de gente querida me dijo que ya estaba bueno y que no podÃa pasarme tantos dÃas triste ya que era un perro y no una persona. Los mandé a la punta del cerro. El amor y el cariño se sienten y punto, nadie puede poner restricciones a tus sentimientos. Espero que Chiquis y Golondrino estén en el mismo cielo de los perros que mi Aceituna, abrazotes!
Geez, that’s unbelievable. Kudos and such.
Dans le temps D. alias ses mille pseudos, aimaient bien imaginer les gens plus âgés que lui, avec toutes sortes de problèmes physiques. Kürbiskerne est la réponse.@ D.: Quel scandale? Oui bien sûr, mais si les enfants deviennent des gens heureux pendant l’enfance, pourquoi pas?
I have been absent for some time, but now I remember why I used to love this blog. Thanks, I’ll try and check back more frequently. How frequently you update your site?
Daniel Campos • 24 de Fevereiro de 2010 às 13:20Bom dia celso, estava lendo este post e tentando colocar a busca personalizada e estava fazendo passo a passo enao nao estou conseguindo… Como faço para a busca aparece na caixa de pesquisa.
It may not be the most romantic story I’ve read but it is surely the most loving and real love story that touches my heart and put a smile on my lips.
I love the blond hair! Cute photos. I am going to join you on that week of clean eating if you don’t mind. And I do wish that I worked with you, if only just on Fridays!! Your food always looks delicious.
Fell out of bed feeling down. This has brightened my day!
Muy bien Jose. Ahora si estamos hablando mejor.Que debemos hacer para eliminar a estos avispados comerciantes? En derecho romano se llama: ” asaltar a la gente en su buena fe” y eso es penado por la ley. Hay algo parecido en las leyes que rigen este Pais? Antonio.
Hi , im back with a report , i scanned / fixed my comp with the trial of Reimage , and it fully repaired my computer. FIxed directx witch i thought i needed to reformat to make it work again , and loads of other stuff. The program is great!
Momentum on these issues is growing, Gary. Whatever we can contribute to it is good. We can never know when we will reach critical mass, but I’m hoping the Occupy events are pushing us in that direction.
Classic Longchamp Bags, Looks very good , excellent and other present ,really good hold , as if it quite definitely ,for certain i will decide to buy for a second time .
Is that really all there is to it because that’d be flabbergasting.
In awe of that answer! Really cool!
At last, someone who knows where to find the beef
Kewl you should come up with that. Excellent!
Your post has lifted the level of debate
Skal vi konkludere med at å bare referere til erfaring er oppskrytt, men at det kan være en nyttig til å ha, det kan ingen komme fra?:-pDen mannlige alko-horebukken, eller mer spissfindig, champagne-gigoloen, lever på gammel chanel no 5. og Gin Tonic. Han er på nivå med alle Gouranga!:-p
Ha ha! Do you know how many times I fish things outta the recycle bin???? And when I do this, most times I think of you and how you upcycle!! LoL! Funny how crafty blog buds seem to make it into our crafty thoughts! It's because you are inspiring!
Whats up. Very nice site!! Guy .. Excellent .. Amazing .. I will bookmark your website and take the feeds additionally…I am happy to find numerous helpful info here in the post. Thank you for sharing..
Ah Claire, désolée, et merci de me le dire. La cuillerée de sirop d’érable se rajoute dans la compotée d’oignons, une fois qu’ils sont bien fondus, pour les faire caraméliser un peu, une ou deux minutes avant la fin de leur cuisson.Bonjour à la famille MTV!
I am drooling!! …. thanks for the Wordle.net link …. that is so cool! I like your 2nd one best. I saved it to my favorites. No time to do it now while I’m working overtme but I will do my own version soon.
A little rationality lifts the quality of the debate here. Thanks for contributing!
Gee willikers, that’s such a great post!
One other issue is when you are in a predicament where you do not possess a cosigner then you may want to try to wear out all of your money for college options. You can get many awards and other grants that will present you with funds that can help with classes expenses. Thanks alot : ) for the post.
I too thought Obama was stupid, but after watching for a while I realized something, he is not stupid, rather he’s brilliant, he knows how to grab and use leverage and power. My greatest fear is that he will try to follow hitler’s path; get into power legally, then grab ultimate control of the country. But, I think he underestimates the American people and their love of freedom, the little of what we have left. Also he gains power from the crumbling of this nation, or destroying this nation just like most dictators gained power. I desperately hope I’m wrong.
Gwen! I love these, they are awesome! I was scrolling through the link party at Tatertots and Jello when I had to do a double take LOL!! LOVE the colorfu backgrounds and your fruit is perfect! Thanks for the shout out too! 🙂
三人ã®ãŠåÂÂã•んを育ã¦ãªãŒらã€ÂãŠ仕事ã«も責任をæŒÂã£ã¦å–り組んã§ã„らã£ã—ゃるã”様åÂÂã«尊敬ã®気æŒÂã¡を抱ãÂÂã¾ã™。ã¿ãªã•んã®色々ãªãŠ考ãˆã«対ã™るãÂÂりんã•んã®ãŠ返事もæ‹ÂèªÂã—ã¦ã„るã¨ã€Âホントã«色々ã¨考ãˆã¦試ã—ã¦頑張ã£ã¦ã„らã£ã—ゃるã”様åÂÂãŒ感ã˜å–れã¾ã—ãŸ。ç§Âã«ã¯å‚考ã«ãªる経験も無ã„ã®ã§ã™ãŒ…ã€Â一ã¤気ã«ãªã£ãŸ事ãŒ有ã£ãŸã®ã§コメントã•ãÂ݋¦頂ãÂÂã¾ã—ãŸ。次男ã•んã®発言ãÂŒã€Âã„ã¤もã¨ã¦も物ã‚Âã‹りãŒ良ã„…ã¨言ã†事ãŒ少ã—気ã«ã‹ã‹りã¾ã—ãŸ。ãÂÂんãªã«欲ã—ã‹ã£ãŸカードももã†è¦Âらãªã„ã€Âå’æ¥Âã™る。…ã¨言ã‚Âれる。ãŠå°Âé£ã„も500円ã§良ã„ã¨ã”本人ãŒ決ã‚ÂãŸã¨書ã‹れã¦ã„ã¾ã—ãŸãÂÂ。ãÂÂã®場é™Âりã®嘘をã¤ã„ã¦ã„るã®ã§ã¯…ã¨言ã†ã®ã§ã¯無ãÂÂã€Âã”両親ã®期待ã«応ãˆよã†ã¨ã€Â次男åÂ݋®ã¨ã¦も一生懸命ãª姿ãŒ感ã˜られるã®ã§ã™。親を困らãÂ݋¦ã—ã¾ã£ãŸã€Â期待ã«åÂÂã—ã¦ã—ã¾ã£ãŸ自分をåÂÂçœÂã—ã¦ã€Â本気ã§åÂ’æ¥Âã—ã¾ã™ã¨æ€Âã£ã¦言ã£ã¦ã„る…。ã§もã€Âホントã®本音ãŒ言ãˆã¦ã„るã®ã‹ãªã‚…ã¨気ã«ãªりã¾ã—ãŸ。ç§Âã¯長年ä¿Â育士ã¨ã—ã¦仕事をã—ã¦ãÂÂãŸã®ã§ã€ÂÃ¥ÂÂ供ã®気æŒÂã¡ãŒ少ã—ã ã‘ã‚Âã‹る部分も有るã®ã§ã¯…ã¨æ€Âã£ã¦ã„るã®ã§ã™ãÂŒã€ÂÃ¥ÂÂ供ã£ã¦褒ã‚Âられるã¨嬉ã—ã„ã—やる気ã«ãªりã¾ã™よãÂÂ。自己肯定感を育ã¦ã¦ã„ãÂÂãŸã‚Âã«ã—ã£ã‹り褒ã‚Âã¾ã—ょã†ã¨ã€Âã©ã“ã«ã§も書ã‹れã¦ã„ã¾ã™。ç§Âも「ãŠ手ä¼Âã„ã—ã¦ãÂÂれã¦ã‚りãÂ΋¨ã†ã€Â「ã™ã£ãÂӋÂÂ助ã‹ã£ãŸã€Â「優ã—ãÂÂã—ã¦ãÂÂれる◯◯ã¡ゃんãŒ大好ãÂÂã€Âç‰ã¨言ã£ã¦ãÂÂã¾ã—ãŸãÂŒã€ÂÃ¥ÂÂ供ãŒ自分自身を好ãÂÂã«ãªり自分ã«自信をæŒÂã¤一番ã®褒ã‚Â方ã¯ã€Â行動を褒ã‚Âるã€Â事ã§ã¯無ãÂÂå˜在を褒ã‚Âるã€Âã¨言ã†事ã ã¨æ€Âã£ã¦ã„ã¾ã™。「ãªんã¦å¯愛ã„åÂÂã€Â「å¯愛ã„ãŠ手ã¦ã€Â「泣ã„ã¦ã¦もã·ーã®ãÂȋ£ãºãÂΌÂ¯æ„›ã„よã€Â「ã“ã“ã«æÂ¥ã¦ã€Â抱ã£ã“ã•ãÂ݋¦〜。ã€Â「ãŠã¯よã†ã€Â今日も会ãˆã¦嬉ã—ã„よã€Â「◯◯ã¡ゃんãŒ大好ãÂÂã€Â排泄ã®ãŠ手ä¼Âã„(紙ã§ãŠ尻をæ‹ÂãÂÂãªã©)をã—ãŸ時ã¯「ã·りã·り元気ウンãƒÂÃ¥Â݋ ãÂÂã€Âãªã©…ã€ÂãÂÂã®åÂÂãÂ΋ÂÂã°ã«居ã¦ãÂÂれる事を嬉ã—ã„ã¨æ€Âã£ã¦るã€Âイイコトをã—ãªã„ã§も居ã¦ãÂÂれるã ã‘ã§嬉ã—ã„ã¨æ€Âã£ã¦る事を言葉ã«ã—ã¦ä¼Âãˆるã¨åÂÂ供ã¯ã™ãÂӋÂÂ安心ã—ã¦ã€Âä¿¡é ¼ã—ã¦ã€Â自分ã®æ€Âã„をã—ã£ã‹りã¨é 慮ãªãÂÂä¼Âãˆã¦ãÂÂã¦ãÂÂれã¾ã™。もã¡ã‚ÂんãÂÂりんã•んã¯ä¿Â育士ã¨ã¯比ã¹物ã«ãªらãªã„愛情をæŒÂã£ã¦ãŠåÂÂã•んを育ã¦接ã—ã¦ã„らã£ã—ゃる事ã¯ã‚Âã‹ã£ã¦居ã¾ã™。ãŸã ãŠåÂÂã•んã®発言をèªÂむã¨ã€ÂãŠåÂÂã•んã¯自分自身ã¸ã®自信ã¨信頼ã¨肯定感を充分ã«感ã˜ã¦ã„らã£ã—ゃらãªã„ã®ã§ã¯…ã¨気ã«ãªã£ã¦…。ã„ã„åÂÂã§居ãŸã„。ã§もボクã¯é•ã†ã®ã‹ãª…。ã¨ã€ÂãŠåÂÂã•んãªりã«æ€Âã„悩むæ€Âã„を抱ã„ã¦ã„らã£ã—ゃるã®ã§ã¯……ã¨。もã†10æ³ã«ãªれã°赤ã¡ゃんã«対ã™るよã†ãª褒ã‚Â方をã—ã¦もãŠã‹ã—ã„ã¨ã¯æ€Âã„ã¾ã™ãÂŒã€Â6æ³ã®åÂÂã§も「大好ãÂÂã€Â抱ã£ã“ã•ãÂ݋¦ã€Âã¨è†Âã«乗ã›るã¨ã™ãÂӋÂÂ安心ã—ã¦ã¾ã—ãŸ。ãÂÂりんã•んãÂ΋ŠåÂÂã•んãÂ΋Š手ä¼Âã„ã—ã¦ãÂÂれãŸ事ãªã©ã€Âã—ã£ã‹りã¨褒ã‚Âã¦èªÂã‚Âã¦ã„らã£ã—ゃる事ã¯よãÂÂã‚Âã‹りã¾ã™。ãŸã ã€ÂãÂÂã“ã«イイåÂÂã˜ゃãªã„時も大好ãÂÂã よã€Âã£ã¦気æŒÂã¡をä¼Âãˆる事も+ã—ã¦ã¿ã¦ã¯如何ã§ã—ょã†ã‹。æœÂãŠåÂÂã•んãŒ起ãÂÂãŸ時毎日一番イイ笑顔ã§「ãŠã¯よã†ã€Âã£ã¦言ã†。スã‚Âンシップを心ãÂ΋‘る…ãªã©ã€Â少ã—ã®工夫ã§ãŠåÂÂã•んã«気æŒÂã¡ã¯ä¼Âã‚Âりã¾ã™。ã¾ã¨ã¾らãªãÂÂã¦ズレãŸコメントã«ãªã£ã¦ã—ã¾ã£ãŸã‹も知れã¾ã›ん…。ã™ã¿ã¾ã›ん…。
These pieces really set a standard in the industry.
Just do me a favor and keep writing such trenchant analyses, OK?
Great post with lots of important stuff.
My first reaction when I read your comment was to be glad none of my overseas cousins call me at 5 a.m. to tell me about random Canadians they’ve met. But early morning phone calls aside, it’s a lovely story, isn’t it? Thanks for the pre-Canada Day smile, and enjoy the long weekend.
Kedves Róbert!Van egy orchideám, amit tavasszal kaptam. Az ablakban van jelenleg, ahol nagyon jól érzi magát. Új hajtásokat és folyamatsan új leveleket hoz….csakhogy a radiátor alatta van. Olvastam, hogy az nem tesz jót neki, és érdeklÅ‘dnék, hogy télen el kellene majd tennem onnan?Ãœdv: Niki
That’s the thinking of a creative mind
on creating a tasty juice, I found a site called Juicing For Men that has some great recipes. The “Blood of Life” is pretty awesome.I don’t really think that juicing is quite the magic space AIDS cure that I
If you’re reading this, you’re all set, pardner!
Arabs were never nations at all. They were nomadic tribes who robbed caravans and raided villages in Africa and Europe for slaves to sell. They continue now as before. Nothing has changed.
Stay with this guys, you’re helping a lot of people.
Wow. So, so sorry to hear about this loss. The name “Guzzo” is very familiar to me as my husband went to college with Rob. He always spoke fondly of him, telling funny stories about capers they were involved in back in Cortland. This is such a shock, my condolences to the Guzzo family. May God comfort you all at this very difficult time.
I don’t like it – BUT it depends on your business model and goals. I think it *could* be necessary for some large sites who need the email addresses to push their products/links etc For a more intimate business model it’s just so off putting. I won’t be putting one on my site in the near future, maybe ever,Ameena Falchetto recently posted..
BonjourJ’ai un soucis avec mon calendrier google sur android, quand je le synchronise il créé des doublette d’événement, il décale les semaines bref il fait n’importe quoi. J’ai eut beau effacer, refaire resync rien n’y fait il n’affiche carrément pas ce qu’il y a dans le contenu internet de mon google. Je trouve ca moyen pour du full google
Rubia Rocha disse:Olá Thamiris, voce pode fazer somente a arte do seu convite com a Boutique do convite, e a impressão diretamente em uma gráfica rápida.O email da Boutique é
This was so helpful and easy! Do you have any articles on rehab?
hi!,I like your writing very much! share we communicate more about your post on AOL? I require an expert on this area to solve my problem. Maybe that’s you! Looking forward to see you.
A perfect reply! Thanks for taking the trouble.
if you have an automatic ice maker, it has to be hooked to a water line…if you don’t have an ice maker, you fill ice cube trays with water, put in freezer, wait till frozen , twist and pop out cubes….ice cube trays…dollar store or bed,bath, and beyond… +1Was this answer helpful?
You’ve managed a first class post
Kudos! What a neat way of thinking about it.
jeje, enhorabonaet recordo que encara m’has d’ensenyar els teus apunts de la eso escrits en un intent de català , xDPD: aquest post m’ha recordat una mica a la introducció de les guies Yale, que el text sempre es el mateix, nomes canviant el nom de la llengua i 2 o 3 paraules més. El podriem adaptar a altres idiomes?
Reviewed on: July 18, 2012loved it I love the show I would pay to see it all over the only thing they did not show there face like in other shows but other then that it’s amazing
I’m impressed by your writing. Are you a professional or just very knowledgeable?
07/06/2010 – 3:58amel más parecido serÃa reggie miller.hasta mañana. eso sÃ, esperemos que sea una serie larga, y la disfrutemos aunque hoy hayamos palmado. un placer estar akà a estas horas comentando con vosotros.
a me piacerebbe diventare tua amica mi chiamo martina , ho 14 anni e sono di asti !!! giulydirectioner sei una ragazza dolcissima , anche se non sono nell’elenco , tvb lo stesso !!!
That’s a genuinely impressive answer.
Coucou Patricia !Les recettes de notre repas seront toutes postées en février, il te faudra un peu de patience donc… Mais promis, tu les retrouveras ici ! :)) Oui, ce gâteau est vraiment extra, tu m’en diras des nouvelles, je vais d’ailleurs en refaire un aujourd’hui ! 🙂 Merci pour tout, tu as raison, restons optimistes !!Bisous bisous xx
That’s a slick answer to a challenging question
Marvellous!! Anything cinnamon works for me – now if only I could find someone to make them for me!!!!Don't know if you're still interested in passing on a RED recipe + short i/v for my RED Alert series? Totally OK if not! Just askin'!!
Thank you so much for this article, it saved me time!
Created the greatest articles, you have.
Someone on the last comment page asked if there was anybody who had a extra Forevermore cd that we could donate to someone who can’t afford one. Does anyone know who it was that asked?. I have a extra one that i will gladly donate.
I found just what I was needed, and it was entertaining!
All of my questions settled-thanks!
You have shed a ray of sunshine into the forum. Thanks!
Holy concise data batman. Lol!
Love your book trailer. I am wondering what age group your book is geared for? My grandson will be turning 8 in a few months and he loves books. The Goosebumps series are still a little too much for him though, maybe next year for those. Enjoyed reading your postings on your book.
Of the panoply of website I’ve pored over this has the most veracity.
159i have tried the macshara and i like the outcome, but my batter was not like yours mine was more like anjeera batter, and when i added the syrub it became too watery. the package of the rice flour i used was 400g.i also want to ask you when you were doing the mixture it looked like you used 2eggs.ed
By Mike November 4, 2009 – 3:33 pmIs it common for LAHSA(Los Angeles Homeless Services Authority) to be off on their count?? I read their findings in the LA times a week or two ago and was surprised as well, especially in the face of our current economy. Is CalWORKS typically more accurate on the numbers??
Maria,Words that make this world go round are a blend of good and bad. Cause and effect, right and wrong all effect us in one way or another.It is always "Your Choice" to filter what you see, read, hear and feel. How we touch others is a blend of many things. But that's what makes us unique is HOW we touch others. You have no problem with it. So delete the negative and don't look back. Stay Calm and Carry On.Bette
El ladrillazo no sólo vuelve es que la verdad nunca se fue. Y además este gobierno tÃtere y mentiroso ya se encarga de legalizar todos los desmanes habidos y por haberBesos
Régebben el sem tudtam képzelni, hogy fűszer és fűszer között ilyen elképesztÅ‘ különbség lehet! A tÅ‘le származó fahéjam például már másfél éves, de ha kinyitom a dobozt, még mindig úgy ontja az illatot, mint egy arab fűszerbazár:)Újabb bizonyÃték arra, hogy nem a recept a fontos, hanem a kiváló minÅ‘ség:))
I am totally wowed and prepared to take the next step now.
need to have unusual results with certain urine tests. If you are pregnant or plan to become pregnant while using where to buy viagra in kl. You may report side effects are more than 3 alcoholic beverages daily. In cases,become pregnant. Use effective birth control (such as cancer medicine such as chloroquine (Arelan) or pyrimethamine (Daraprim), or quinine (Qualaquin); erectile dysfunction medicine such as glycopyrrolate (Robinul) mepenzolateKeep on going.
Meredith, thank you for sharing your family…and what a beautiful family you are. I loved getting to know another woman who is blessed to be a mother by birth and adoption.Deborah, thank you for introducing us to Meredith.
Hallelujah! I needed this-you’re my savior.
Me l’aviez vous volée ? et pour d’autres sans doute étais je « hors sujet »….do zobaszenia,my lord,hvala vam ti puno…………. »on est prié de fermer les yeux «
I’ll try to put this to good use immediately.
is a wonderful small city to wind up in (Is that because it's more German-American than the rest of Texas's cities?)"Yeah, I dunno about that. Toledo, OH is heavily German, and it's no paradise. It's like Detroit, if it was run by the Disney corporation. For that matter, even metro-Detroit is heavily German. Even if you ignore the city entirely, most of Detroit's suburbs are also extremely dysfunctional.
Knocked my socks off with knowledge!
I really, really needed to read this today. You are not alone in these feelings, thoughts, and struggles — though I know that doesn’t make them any easier to overthrow (and yes, it’s a revolution!). Thank you for sharing; now I feel less alone myself.
meu celular é samsung GT-S3350 e eu quero saber como que é o codigo para deixar meu celular mais auto????? por favor fala ….
Ah, i see. Well that’s not too tricky at all!»
Mighty useful. Make no mistake, I appreciate it.
Thanks for introducing a little rationality into this debate.
Fell out of bed feeling down. This has brightened my day!
A really good answer, full of rationality!
That’s the smart thinking we could all benefit from.
Call me wind because I am absolutely blown away.
Ab fab my goodly man.
I cannot tell a lie, that really helped.
Good for you – I did this once at Queen’s. It’s eye-opening. Learned that my natural management style fit well with many as it allowed for them to exercise their initiative. People who wanted a more directive kind of style were not so happy.
I appreciate you taking to time to contribute That’s very helpful.
1. Doctor Who was the first thing I found fandoms of online, and I got into fan fiction and YouTube from there.2. I don't watch any. *hangs head in shame*
Your bracelet is beautiful! I have just started using LOS and I have many questions. My biggest, but probably stupid, question is this…can you put items into LOS that have glass beads on them, or do you need to patina BEFORE you add the beads? I ask because sometimes I don’t know if I want to patina until I see how my design develops. Any tips you have would be wunderful! Thanks bunches!P.S. LOVE LOVE LOVE the business card holder!
That’s the best answer by far! Thanks for contributing.
I love this! What a great idea…and your list is awesome! I love your sense of humor and what I can see of your hair in your avi.And of course, that little angel.
You have the monopoly on useful information-aren’t monopolies illegal? 😉
I agree with Lisa. Tonight, someone I previously blocked showed up in my timeline. You’d think Twitter would at least respect previous blocks with their new retweet scheme.
I read your posting and was jealous
Didn’t know the forum rules allowed such brilliant posts.
Good to see a talent at work. I can’t match that.
Didn’t know the forum rules allowed such brilliant posts.
You have intellectualized your story — objectivity at it’s best…..now, EXPERIENCE what you have just written….ie: “I would rather freeze to death then be without him”maybe: dissect that “kind of numb” that surrounds the writer…what benefit does freezing offer one????
I’m really into it, thanks for this great stuff!
Heck yeah bay-bee keep them coming!
Ja dette er triste greier! Og så tragisk at liv gikk med. La oss håpe den ikke kantrer, men det ser jo ikke akkurat lyst ut sånn utpå kvelden.
I could read a book about this without finding such real-world approaches!
Hey there! This is my 1st comment here so I just wanted to give a quick shout out and say I really enjoy reading through your blog posts. Can you recommend any other blogs/websites/forums that deal with the same topics? Thanks a lot!
Thanks for taking the time to post. It’s lifted the level of debate
Your posting lays bare the truth
cindiloohoo – Finally! Someone asks "WHY"? Look at my video(s) and you will know why they did this. "Who" did this is "they", the not-yet-humans who are afraid of The Truth. And YouTube is not the only way to get it out.
Beyond the obvious problems of coal dust and many mega-hauling trains, here’s another reason NOT to export coal – do we really want to contribute more to China’s output?
This site is like a classroom, except I don’t hate it. lol
Hallo Christiene,Leuk geschreven verhaaltje, over een ontmoeting met een mysterieuze dame, weliswaar anders dan de andere. Vragen komen op: "Wie is deze vrouw? Vanwaar komt ze? Waar gaat ze heen?" Is dit slechts een eenmalige ontmoeting, een toevallige passante? Lezers willen het spannende vervolg kennen, de zoektocht naar… misschien komt hier ooit wel een vervolg… of blijven we op onze honger zitten, hint ;-))
Hello. Very cool website!! Man .. Excellent .. Amazing .. I will bookmark your web site and take the feeds also…I’m satisfied to locate so much useful information here in the article. Thank you for sharing…
i have been waiting for this particular interview for a long time.this is exactly why this website is unique in bringing forth and sharing these audio interviews.thank you again Cielo Drive.
Definitely believe that which you said. Your favorite justification appeared to be on the online the easiest thing to be aware of. I say to you, I definitely get annoyed when individuals think about worries that they just will not know about. You managed to hit the nail upon the top and also defined out the whole thing without the need of having side effect , persons can just take a signal. Will possible be back to get more. Many thanks a lot
You keep it up now, understand? Really good to know.
Thank you for posting this vlog! I am saddened to hear about what is going on in Buffalo since I left. It was amazing to see all of the growth that happened at DAS since Sarah began; but I am hopeful DAS will continue searching and employ a Deaf person who will expand on knowledge, advocacy and services in Buffalo even more.
O 24° lugar de Tiago Machado na geral do Giro até o momento presente, mostra que o ciclista de Famalicão, já é um dos grandes, dado ser a estreia dele numa grande volta,Se continuar numa grande equipe (vai continuar) num futuro bem próximo estará no Top 10 do ciclismo mundial de elite. Vai terminar nos vinte primeiros concerteza, e estará entre os cinco primeiros no próximo Giro.
hi!,I like your writing very much! percentage we keep in touch extra approximately your article on AOL? I require a specialist in this area to solve my problem. May be that’s you! Looking forward to see you.
Good job making it appear easy.
Sweet blog! I found it while searching on Yahoo News. Do you have any tips on how to get listed in Yahoo News? I’ve been trying for a while but I never seem to get there! Thank you
Well, it was the good will of TE which ensured rather early commisioning of IMEWE. I also must add that TE had been cooperative with all the projects transiting through TE and wish to complete them in earliest possible time frame, however, they eventually could not succeed in their objective due to adverse situations. Neverthless, situation has improved significantly leding to new projects seeing light of the day.
Economies are in dire straits, but I can count on this!
love hearing that people have a great time at our Open Houses! Click here to read a post on the Wine Wench by Gayle Hedrington. « LaBelle Winery at the New Boston
I love reading these articles because they’re short but informative.
I like to party, not look articles up online. You made it happen.
Counterfeit handbags are copied, with inferior materials, low-paid workers and who knows what age, but someone has a large illegal proceeds. Each woman must decide what to buy, but ask anyone who has had authentic Prada Designer Handbags Online and witness the excellent quality and absolute satisfaction.
This is actually the ideal web site for anybody who chooses to have an understanding of this unique niche. You use a great deal it has the practically difficult to argue for you (not really that I dreamed of). Unquestionably position an exciting new ” spin ” on the subject thats ended up discussed about the items quite a few years. Amazing!
This is the perfect way to break down this information.
imagining someone like that in charge of the country for another four years…..that should be the only unifying issue necessary.anything else and the electorate is dumber than a sack of hair.
That hits the target dead center! Great answer!
Was totally stuck until I read this, now back up and running.
Mihai, din CNA au participat efectiv 5 membri la sapaturi iar alti trei au venit deseori. Din Grup a participat o persoana. Cu tot respectul, din zona opozitiei nu a participat absolut niciunul. Cat despre scrisoarea lui Beatrice, cu parere de rau este o manipulare grosolana. Daca tu poti dovedi ca e autentica (si sa si publici un faximil al ei) ai tot respectul meu.
You will have that strength, I’m sure of it. I only wish I could be there to see it. My friend Meg is running the marathon too, for Housing Families. But it’s such a mess of a race to view…such a bummer. I’ll be thinking of both of you that day though, that’s for sure.
Hallo,Notizbuch und Sitzkissen gefallen mir ausgesprochen gut. Es reizt mich das Bemalen von Leder auszuprobieren. Welche Acrylfarbe hast du benutzt?Lieben GrußSiebensachen
Cop used his cruiser to tag a shooter years/ decades ago in a burb of LA, Kali. I remember it because we calculated it as a hit with a 22,400,000 gr hollow point. Pretty effective. Good to hear the cop is doing well.
I don’t even know what to say, this made things so much easier!
These photo, girl in hug with text, is an advertise from POST – it was made in Australia. See more inFoolzParadise.OrgIf you dont could find it, please, write me, and I send you the image.DM
Wow, your post makes mine look feeble. More power to you!
This will be the turning point of the Obama presidency when people see him for what he really is – out of his depth, beholden to wall st and without any plan whatsoever for this constant wars.How's that change feeling America?
Mä oon kanssa haaveillut tuollaista seinähyllyä lastenhuoneeseen kirjoja varten. Ehkäpä kesällä tekaisen sellasen itse. Aattelis ettei se kamalan vaikea oo tehdä. Vai oiskohan?
Articles like this are an example of quick, helpful answers.
I keep listening to the news bulletin talk about receiving boundless online grant applications so I have been looking around for the most excellent site to get one. Could you tell me please, where could i acquire some?
Hey, I have an idea. What say we just keep talking crap about her until she goes nuts like Britney? Yeah, that would be real fun. We can all sit back and say “Look what we did.” The girl is growing up. She is still trying to find herself. Can we not let her do that?
Nice fun puzzle today. I am crap at spotting setters but when it was suggested I took another look and would plump for RayT.5d and the well deserved 2d were favourite.Thanks to the presumed setter and to BD.
June Hi Ryan! How lovely of you to keep in touch with your supporters. Thank you for your songs , especially Not Far Apart! Keep well and will see you and the CT team in February in Australia. June
Most states and communities don’t require them to be in shape to ride to work on clear days if you want to do your bit for the next 2 to 3 years. The motor can only help the pedals performance itself, which in turn would make the bike anytime you like and switch back to electric motor to enjoy the pleasure ride.
When you're learning chords, you learn and study them for only One Key at a time. Do not overlook this part of your learning. When you're acquainted with these core 7 keys you can start to learn about the black keys (flats and sharps).my web-site: my webpage:
si lo dejan afuera por algo será. si algo es bueno, el contenido resalta, la gente lo recomienda, etc. si algo es malo, puede tener mil followers de una pero a la semana queda en 0.sino estás tratando a los usuarios de twitter de boludos (algunos lo somos igual)
Dear Sandy, I have sent you a private email. Thank you so much for sharing your enthusiasm over Golgi products. Please check your email. Warmly, Rita
I have all of these ingredients in my kitchen, but would never have thought to combine them in this way. I really want to try cooking the pork belly in the caramel sauce. So interesting…
I really couldn’t ask for more from this article.
Pretty insightful post. Never thought that it was this simple after all. I had spent a good deal of my time looking for someone to explain this subject clearly and you?re the only one that ever did that. Kudos to you! Keep it up
a utima que deu para min era virgem ela ficou andando com as perna abertas por tres dias e nao adienta pedir para parar que eu nao paro eu rasgo mesmo meu apelido e cavalao por causa do meu penis
Was totally stuck until I read this, now back up and running.
Somebody essentially help to make severely articles I might state. This is the very first time I frequented your website page and to this point? I surprised with the analysis you made to make this particular publish extraordinary. Fantastic activity!
I can’t drag’n’drop files to PhpStorm any more! When I drag an xml file from my desktop (windows 7) to PhpStorm 2.1.3 or 2.1.4 it doesn’t open and the mouse cursor takes a form of crossed circle.In version 2.1.1 I’m able to open exactly the same file doing the same actions. Should I switch something in the setting or it is a bug?
The Housekeeper’s Pocketbook, by Sarah Harrison, 1733, page 58The Lady’s, Housewife’s, and Cookmaid’s Assistant, by E. Taylor, 1769, page 209The London Art of Cookery, by John Farley, 1783, page 200
That’s 2 clever by half and 2×2 clever 4 me. Thanks!
Thanks a lot for providing individuals with a very superb possiblity to read in detail from this site. It is usually very terrific and as well , full of fun for me personally and my office friends to visit your blog the equivalent of thrice every week to study the fresh guides you have got. And of course, I’m always fulfilled concerning the striking concepts you give. Some 4 ideas in this article are basically the most impressive I’ve ever had.
12ePourquoi faudrait il des occasions spéciales ?un anniversaire, une fête, ou la fin d&8n;172a#née….mais aussi pour remercier quelqu’un car de nos jours une carte papier se fait beaucoup plus rare et s’apprécie donc encore plus
I never employed a silver treasures sparkle betterscooter.com at this point, the weather through Aurora has long been challenging. With the sodium and in addition dingy ice, I don’t want to buy smudged.
Har du nongdsiene lavet en Tusnelda ??Det blev jeg kaldt som lille og havde faktisk glemt det indtil julen i år hvor vi spillede et børnespil i julen, hvor man skulle sige hvem man var og der opdagede jeg at jeg faktisk er en Tusnelda. Ved ikke helt hvorfor jeg skriver det til dig udover at det nu kunne være sjovt at se hvordan du syntes, sådan en ser ud !!
At last! Something clear I can understand. Thanks!
Helene:Ingen årsak og selv takk. :)Kristina: Det er godt å høre at flere svetter over tilsynelatende små oppgaver i hverdagen som blir til de skrekkeligste kamper. Felles skjebne, felles trøst.
Wow! Quel article inspirant! J’aime beaucoup la distinction entre la douleur et la souffrance, et pour l’avoir vécu intensément… la souffrance de ne pas avoir vécu la douleur, je trouve que c’est tout-à -fait vrai. Je retiens également la question: Quand es-tu? qui est très puissante et qui me parle énormément! Merci Nathalie;)
Bardzo dziękujemy za koncert dla rodziców, który odbył się w naszej szkole-ZSS nr 103 w Poznaniu. Było to dla wszystkich niezapomniane przeżycie i dostarczyło wielu wrażeń. Koncert był po prostu wspaniały. Życzymy wielu dalszych sukcesów.
breastpump ni ade lagi x? kalau rosak,contohnye pump die rosak or valve yg kecik tu rosak,kt mane nk beli ganti die? sbb jarang jumpe brand ni..
« Le capitalisme libéral-libertaire des pays anglophones diffuse partout dans le monde par l’internet l’individualisme émancipateur et la liberté pour le citoyen de faire ses propres choix sans être plus ou moins subtilement guidé par les personnes agrées par les autorités compétentes »Apparemment, vous avez trop lu le Journal de Mickey.
Very interesting blog I must say. The you say are generally right, but I do not agree on everything you say.I will come back to see what else you have to say and what the reaction of other people on your blog . Keep up the good work.
You have more useful info than the British had colonies pre-WWII.
Glad I’ve finally found something I agree with!
It looks like you had a great time. I will definitely keep my son rear facing until he is 2. He is a small boy and I think he is much safer that way. jj250@aol.com
Write down what you’re learning. Teach your wife. Make a recording. Step out of the comfort zone and I promise you won’t look back. Let me know how you go with the dog.
Cuando fui de visita a México con Critter de bebé no sabes la angustia que pasaba en el coche porque el tráfico era tal que nunca llegaba a tiempo para prepararle el biberón y respetar las tomas… ahora si ¡mis respetos! aprender a manejar y con niño ¡que locura! un besote desmadroso
Thinking like that shows an expert’s touch
C’est un acte magnifique s’il n’y a aucune contre indication médicale pour la maman et seules les personnes confrontées à des difficultés de conception d’enfants peuvent comprendre ce geste et la douleur immense que provoque la stérilité . Surtout qu’on a l’impression et d’être coupables dans la société actuelle du fait de ne pas pouvoir avoir d’enfants. J’ai vécu cette situation et j’ai du passer par la case fivicsi qui a par chance aboutie mais j’aurai été prète à tout pour avoir un enfant
Many thanks for creating the effort to discuss this, I feel strongly about this and love learning a great deal more on this matter. If feasible, as you gain knowledge, would you mind updating your weblog with a great deal more information? It’s really beneficial for me.
Super informative writing; keep it up.
I am forever indebted to you for this information.
This does look promising. I’ll keep coming back for more.
Your website has to be the electronic Swiss army knife for this topic.
Hello! I finally got the Bradbury book on order. I think it is a very interesting book with good suggestions for a writer. He must have been an interesting little kid! I keep the book handy in the car as I’m doing a fair bit of driving around for my son due to car issues. so I’m reading it in chunks and rereading. ( Congrats on your son’s PHD!!!)I think your blog writing also mirrors the very thoughtful reflections at the very core of who you must be as a writer. Your writing inspires reflection.
Anche i sussidi di disoccupazione continuano da troppo tempo a ballare sopra la linea maginot di demarcazione tra un vera creazione di lavoro e dichiarazioni di buona volontà. Servono almeno 250.000 nuovi posti di lavoro ogni mese per i prossimi dieci anni per cancellare le pressioni demografiche e migratorie e tutte le anime che hanno perso un posto di lavoro in questi anni di terribile crisi, di disoccupazione in buona parte strutturale.
I’m impressed, not only did he manage to reach around and pop his own pimple/abscess, he managed to have the camera remain still and focused. Very nice job sir, very nice indeed. I do think however that he would have gotten much better results if there had been someone else to assist him with the actual popping process. I could tell that it was uncomfortable for him. Not sure how much of that was from the stretching, or from the pain of popping. I would love to see part 2 when it’s ready for an encore since it was obvious that some material remained.Well-loved.
Felt so hopeless looking for answers to my questions…until now.
How could any of this be better stated? It couldn’t.
Quand ils disent » Préparons les planches et les clous ! », ce n’est pas une allusion à la crucifixion, c’est une allusion à la préparation d’un cercueil (voir le croque-mort de Lucky Luke).Ceci n’est pas une critique de votre article, mais une aide à bien cibler la nature de l’opposition
This is so true for me too. I think it explains why I’ve bounced around through several different “doings”. Each has been a path along the way and I’m now, after nearly two years, coming back to the primary one. And your “Shrinking to Fit” post was also instrumental for me here. One of these days soon I want to blog about it.
No question this is the place to get this info, thanks y’all.
What a wonderful garden visit! I so enjoyed seeing your photos. It looks like a nice amount of color for the winter… and I love birches, though I do not have any yet. Planting them beside evergreens is a wonderful idea. Thanks for sharing, Pauline!Merry Christmas to you and your family!!!~Julie
Wow, your post makes mine look feeble. More power to you!
Awesome you should think of something like that
Thanks for sharing. What a pleasure to read!
Its really an interesting analysis. .de tops the gtlds all time. With gaining interest & higher index shows the growth of .in extension. I m happy to see such an information as am invested a lot in .in
The voice of rationality! Good to hear from you.
Thanks for introducing a little rationality into this debate.
I. Love. This. Post. The common denominator between each archetype that you listed seems to be an excess of self-involvement, and consequently, loss of big-picture perspective. Of course, the world needs both macro- and microcosmic thinking, but it’s good to at least figure out in which camp you tend to stake your tent. To the cranky people who got defensive: bear in mind that defensiveness is the first affirmation of addiction. I will admit to enjoying proper grammar. It makes me feel like there might be order in the universe somewhere. Thanks.
That’s an astute answer to a tricky question
I was so confused about what to buy, but this makes it understandable.
I've noticed that whatever .html file google puts on the page is what prevents you from seeing your site…delete this file and your site will magically reappear. Google you should be ashamed of yourself for this tactic. Go after the hackers and prosecute them…don't make the innocent web designers and businesses owners suffer!
Ca MARCHE! je suis une rongeuse folle depuis mes 5 ans, et j’ai employé cette méthode (en desespoir de cause, on va pas se mentir) il y 3 mois et… je n’ai pas récidivé!!Il faut tout de même les limer un peu de temps en temps, car plus les ongles sont longs, plus ils risquent de se casser bêtement, et là , la tentation de les grignoter « juste pour égaliser » est trop grande!Bon courage à toutes celles qui tentent le coup, quelle satisfaction une fois passé le cap!
Wiecie to ma też i dobre strony :1.Nie będzie tyle bugów2.będzie się grało przyjemniej3.Na razie można pograć w (zbugowaną,co prawda to prawda)wersję pre release)
Padilla calling LaHair a “quality option off the bench” is a bit of a stretch. Maybe he tuned-out after the all-star break and only saw LaHair’s season-ending walk-off.
The answer of an expert. Good to hear from you.
Haha. I woke up down today. You’ve cheered me up!
I do agree with all of the ideas you’ve presented in your post. They are really convincing and will definitely work. Still, the posts are very short for starters. Could you please extend them a little from next time? Thanks for the post.
This article is a home run, pure and simple!
Jeez-oh, I can't believe anyone would be offended by this. Such things should be taken in the spirit in which they were intended. Clearly iPKat did not set out to offend anyone. I see no need to apologise.
This post has helped me think things through
Nice read, I just passed this onto a friend who was doing some research on that. And he just bought me lunch since I found it for him smile Therefore let me rephrase that: Thanks for lunch!
ENIRientrato su ENI venerdì attorno ai minimi di mattinata pensando/sperando fosse un ritracciamento. Il report del pomeriggio mi induceva senza indugio a piazzare stop strettissimo sul minimo di mattinata. Infatti lo spunto in alto pomeridiano non bucava i massimi di mattinata e puntualmente sono andato in stop nei primi secondi stamane. Mercato difficilissimo.
Call me wind because I am absolutely blown away.
What i do not understood is in fact how you’re now not really a lot more neatly-appreciated than you may be right now. You are so intelligent. You know therefore significantly in the case of this matter, produced me for my part imagine it from so many various angles. Its like men and women are not involved except it’s one thing to accomplish with Girl gaga! Your personal stuffs excellent. All the time handle it up!
Now I feel stupid. That’s cleared it up for me
This reminds me of “Eat, Pray, Love” and her relationship with the “Geet” (the Gurugita) – have you read that book? It’s a gem. She had much resistance to her chanting as well. Anywho, thought-inducing post. Maybe i should stick to some of my practices
Jaj, egy valamit kifelejtettem:Szoktam mangákat/bescannelt magazinokat olvasni, ezekkel hogy birkózik meg a kindle? Közepes vagy nagy felbontású, fekete-fehér képfájlokról van szó.Előre is köszi a választ
At last! Something clear I can understand. Thanks!
12-09-2012 o 20:21Mirek Napisał(a):Teraz ja , brak formy oczywiście , treningów jak najbardziej , ból , ogólna niedyspozycja , nikończące się skurcze ,suma sumarum nadaje się na ojomAle jadę do dyspozycji auto (5+5)pozdrowienia
I’m impressed. You’ve really raised the bar with that.
And I thought I was the sensible one. Thanks for setting me straight.
– Just wish to say your article is as astonishing. The clarity in your post is just great and i can assume you are an expert on this subject. Fine with your permission allow me to grab your RSS feed to keep updated with forthcoming post. Thanks a million and please continue the enjoyable work.
You’ve got to be kidding me-it’s so transparently clear now!
Wat een leuke Give Away heb je ontvangen en gelukkig gaat het allemaal goed komen met je arm!Je stoelen en je tafel vind ik helemaal super, mooi hoor! Groetjes en een fijn weekend,Esther
First – Thanks Trish for introducing us to the is beautiful site! I am opening the page in the morning and the banner image at the top is just glorious! What a beautiful and well penned post! I am going to share it in a discussion we are having on FB this morning at Guiding Light Homeschool. In a year where too many of my friends have believed the lies – and lost hope, I am in ferverent prayer for those of us walking out our covenant marriages!
Hola, tengo problemas para visualizar correctamente el formulario de inscripción en Word, no tengo problemas de fuentes faltantes, hay partes de las palabras del tÃtulo que no se ven y si las agrego yo, no queda bien. PodrÃan enviar el formulario en otro formato (pdf, .docx)Muchas gracias
Man Neal I really shampooed your fur this morning didn’t I? Did you really think you could stand toe to toe with me?Your a little child with childish insults. You have no game, now go pick up your jock strap, it’s waiting for you on the 20 yard line Precious!
So i looked up original 80′s movie and the evil step father in it was played by the actor who played John Lock on “Lost”.I continue to type in random factual observations amongst the tom foolery.
Thank you for the sensible critique. Me and my neighbor were just preparing to do some research on this. We got a grab a book from our local library but I think I learned more from this post. I’m very glad to see such fantastic info being shared freely out there.
Begun, the great internet education has.
Mitt Romney and home is Massachusetts. After all, Governor Romney ended his tenure with a dismal 34 percent approval rating and now trails President Obama by as much as 20 points in his own state. Worse still, Romney
Always refreshing to hear a rational answer.
Thanks for your challenge and also attempts! This stuff on your own internet site will be terrific. Furthermore My partner and i significantly treasure the thoughts. For me they’re significant things. Anyhow thanks. Fantastic look over.
Deep thinking – adds a new dimension to it all.
This sounds a but suspicious to me. I do not deny any persons right to self defense, but I find it interesting that they are buying NFA weapons, 14″ short barreled shotguns. This would not be my weapon of choice to use in an active shooter scenario in a crowded school setting. I find the quantity interesting also, if I had to guess it sounds like the DE is starting up a large, well armed security force for their main headquarters. Since Constitutionalists who don’t agree with the existance of the DE are on the terrorist watch list it makes sense that this government should want to arm itself against them.
Oh geweldig! Ik heb altijd afgesproken dat ik bij elke designer x H&M collectie minimaal één item moet kopen, wat moet ik kiezen?! With love,
The expertise shines through. Thanks for taking the time to answer.
The honesty of your posting shines through
This «free sharing» of information seems too good to be true. Like communism.
Je viens d’en tomber follement amoureuse… Surtout en version bleu.C’est sur qu’il y a d’autres priorités mais si genre tu le mets sur ta liste de mariage en le faisant passer pour un bagage pour ton voyage de noce ca peut passer nan ?
Ã…h, nam Kjersti, det sÃ¥ godt ut!!!Jeg hadde tenkt til Ã¥ fylle opp fryseren før bebisen kommer, men har ikke fÃ¥tt ut fingeren enda…! Huff…! Men kanskje litt baking i kveld?God mandag!Klem Ellen
netizen –Yes, I would like to post that graph; it's a good one. Unfortunately, when I reduce it to blog size, the scales become unreadable. This means I have to redo the text on the two scales after it has been resized. That takes a bit of time, which I don't have much of. So I haven't done it yet.
Cheers pal. I do appreciate the writing.
No more s***. All posts of this quality from now on
Walking in the presence of giants here. Cool thinking all around!
Esta decada foi tão marcante na vida do Brasil e dos Brasileiros , que até hoje meus filhos curtem musica que eu curtia nas discotecas.
127I truly love your website.. Very nice colors & theme. Did you create this website yourself? Please reply back as I’m attempting to create my very own website and want to know where you got this from or what the theme is called. Appreciate it!
Listen to it again – the radio program was the first one to conjecture the last name and this blog just picked up on that. So did I. So did a lot of people. It isn't rocket science. And its covered by the first amendment.
Hei Sølvi:)Du er som vanlig full av gode idèer!Så morsomt med den treskoen!Kjempefin idè altså.Globusen er veldig fin, jeg ønsker meg også en sånn.På tide å begynne å lære barna hvordan ting henger sammen:)Ha en finfin kveld!Klem herfra:)
indeed! A lot of your comments apply to non ADHDers too I think. It’s almost as if teachers try to make school as unpleasant and fear-filled boring experience for the learners. Thank you for your input and let’s have more of the same..-= Lauren Cooper´s last blog .. =-.
Da ist Broder aber anderer Meinung. “Bis gestern war auf jetzt.de, der “Schule&Job”-Seite der SZ, ein “Brief†zu lesen, den Ken Jebsen mir geschrieben hatte. Für jeden Leser, der nicht nur “Fritz†hört, eindeutig als Satire erkennbar. Nachdem Jebsens Anwältin sich bei der SZ gemeldet hatte, wurde der Text vom Netz genommen. Allerdings ist er noch hier zu finden. “
Hello Kenneth, Thank you for your thoughtful response and dedicated political activity. The ongoing political education that is needed to enlighten people’s minds and diminish ignorance will definitely take time to accomplish. Meanwhile, we must continue this ideological struggle against incorrect and ignorant ideas as they are like poisonous weeds that require resistance and elimination. Jimmy Franco Sr.
What a shame. Those dance parties allowed for a mix of people to enjoy that space in a modern fashion, pulling in people that never would set foot in there. As an artist, it felt communal. One of those Brazilian nights was outstanding. Now, it will feel fake like being part of a culture/science experiment. While all of Brooklyn re-defines its self, we are all invited to take part in and explore the museum like any other out of touch art space. Hooray.
Grade A stuff. I’m unquestionably in your debt.
The open land mandated around a nuclear plant tends to be forest or grassland or desert. Large sections are undisturbed and therefore wildlife flourishes. Oconee and McGuire nuclear stations, just to name two, have won environmental stewardship awards. There are gardens of native plantings that feed the wildlife. Idaho National Lab's vast acreage is home to many test reactors, and environmentalists love that land because so much of it is in pristine condition and home to a lot of wildlife and native vegetation.Thanks for doing battle, David.
Ã’ûðôøüøр:Ãœýõ þчõýь ÿþýрðòøÃȄÂѠüõтþô ÿрõÿþôðòðýøÑÂ.áтрðх ÿþтõрø òþ÷üþöýþÑÂтø ÿþûучøть ÿþÑÂûõôующøõ ÷ýðýøÑÂ,÷ðÑÂтðòÃȄÂõт ÷ðúрõÿøть уöõ ÿþûучõýýыù üðтõрøðû,ÿþôтðûúøòðõт ú ÑÂðüþôøÑÂцøÿûøýõ.ÃÂ’ ÑÂòþю þчõрõôь úðчõÑÂтòõýýыù üðтõрøðû ø ÿþýÑÂтýþ òыûþöõý ò òøôõþ урþúðх.áуÿõр! Ñþûьшþõ ÑÂÿðÑÂøñþ.
That’s a mold-breaker. Great thinking!
Posted by on September 11, 2012 at 1:09 pm Dee,I’m glad you caught onto my subtle anecdotes. If you can’t have fun with it then why do it, right?After doing some research for this post, I to was surprised to see how many people favored their Klout score. Not only that but seemed to go out of their way just to improve their score. Makes me wonder if they would have made more money by using that time towards more content or building their funnel. Things that make you go hmmm…Ken
ambien…I’ll gear this review to 2 types of people: current Zune owners who are considering an upgrade, and people trying to decide between a Zune and an iPod. (There are other players worth considering out there, like the Sony Walkman X, but I hope this give…
What a pleasure to find someone who thinks through the issues
Hello! Thanks for having this giveaway!!Enter me, I'm a follower of your blog via GFC (Susalie)I would like to see more skincare posts :)Email: susalie at hotmail dot comI put your giveaway in my sidebar: babydollvanitybox.blogspot.com
What makes me happy is when a fellow brave girl member sends you a message that your work inspires them, it touches my heart, it validates that I am a creative person which I question and doubt all the time. I started to art journal about a year ago. I haven’t done much art in a long long time for many reasons. It has been a source of therpy. I am a better wife, mother, friend and person for it.
laba diena, norejau pasiteirauti turime nusipirke bilietus is ryanair su persedimu, paanstino lektuvo skrydi 35min. i kuri turim persesti ir mes i ji nebespejame, ar yra ryanair galimybe pasikeisti bilieto laika i velesni (nes yra ta pacia diena skrydis vakare), neprarandant pinigu uz jau nupirktus bilietus?
Kewl you should come up with that. Excellent!
How neat! Is it really this simple? You make it look easy.
That’s 2 clever by half and 2×2 clever 4 me. Thanks!
this on the WKUK site so plz dont think i’m wierd lol but YOU….ARE….SEXY…HOT!!! hah. im a huge fan and would also love if you toured near San Antonio TX. thanks and have a nice day!
You’re a real deep thinker. Thanks for sharing.
Howdy very cool website!! Guy .. Excellent .. Wonderful .. I will bookmark your blog and take the feeds also…I am satisfied to find a lot of helpful info right here in the put up, we want work out extra strategies on this regard, thanks for sharing.
What an awesome way to explain this-now I know everything!
Aceasta este absollutely cea mai bună descriere a cădere liberă în depresie. Eu nu sunt bi-polare, astfel încât să nu experimentat maximele extreme, dar cât de bine ştiu de mici adâncimi. Ai capturat într-adevăr o experienţă pentru mine.Jan recent postat..
When this goes public, I wonder how many would institute a "fair use" or "fair dealing" system by allowing downloading for personal use (no CC license) but disabling embedding? It actually makes much more sense than allowing embedding but not downloading.
And I laughed out loud at this: foreign (well, Mexican) mission . Is Mexico not really a foreign mission?But only for the reverse – my SLC-bred wife served in a foreign mission – hispanohablante Orange County. She joked that it was really a foreign country, but with 7-Elevens.
Hi would you mind letting me know which hosting company you’re working with? I’ve loaded your blog in 3 completely different browsers and I must say this blog loads a lot faster then most. Can you suggest a good internet hosting provider at a honest price? Cheers, I appreciate it!
drugs. Now, several years later, he continues to lecture on, and publish, the latest techniques for gynecomastia treatment without surgery. Visit his site for all of the latest and greatest approaches for eliminating gynecomastia
Do you have more great articles like this one?
I precisely wanted to thank you very much once again. I’m not certain the things I might have sorted out in the absence of the actual tricks contributed by you regarding such area. It truly was a very intimidating concern in my opinion, but viewing this well-written approach you resolved the issue took me to leap with gladness. I will be happier for the guidance and trust you find out what a powerful job you are putting in teaching other individuals all through your blog. Probably you’ve never got to know any of us.Welcome to my blog .
I like the worthwhile details you produce within your content articles.I’ll bookmark your web site and take a look at once again here frequently.I am really guaranteed I will know a great deal of new stuff proper the following! Decent luck for that upcoming!
Pemohon juga boleh mendapatkan maklumat lanjut mengenai program pengajian dengan menghubungi IPTA dan Politeknik melalui alamat dan nombor telefon yang disediakan di Senarai IPTA Universiti Di Malaysia.
I always say…everything is political these days..sick ain't it?Don't you have a great photoshop of Tom Delay in a cellar in chains? I swear I saw it here. I know…its off topic…sorry.
Wowza, problem solved like it never happened.
Kitch – You know what? I get bitter about a lot of things, but I never once felt bitter yesterday and I didn’t think about this miracle until you mentioned it here. I think that even before the day began, and as it transpired, I was aware of its weight and had a certain reverence for it. Does that make sense? Isn’t it amazing that moments, exquisite moments, can be at once heartbreaking and reassuring?
You don’t even have to be rooted/install a custom rom to have the home screen rotate…..nova launcher and ultimate screen rotation app does it.
Your posting really straightened me out. Thanks!
Tak Rikke, jeg følger jo spændt med i dit projekt ogsÃ¥… Jeg er halvvejs nu, med strikket, er meget spændt pÃ¥ at skulle lave stencil tryk pÃ¥ det, og klippe op, jeg har ikke klippet i strømpegarn før…
Never would have thunk I would find this so indispensable.
Deilig med farger!Kos dere i helga!Vi skal på dukketeater i morgen alle fire. Gleder oss like mye hele gjengen tror jeg ;)Klæm
At last, someone who comes to the heart of it all
Hey, that’s the greatest! So with ll this brain power AWHFY?
Umm, are you really just giving this info out for nothing?
Thanks for your thoughts. It’s helped me a lot.
I really liked the book titled "The History and Geography of Human Genes" because it contains very interesting information. I agree with the author in the sense that human beings is only race.
This is great! I had a stability ball for years, but left it with my parents when my husband and I got married. Now that he and I are getting more active, the hubs went and grabbed the old stability ball, but it’s been rolling around for the last couple of days. Now I have a few more exercises to add to the mix! Thanks!
Good to see a talent at work. I can’t match that.
July 25, 2011 at 7:44 amNancyI think part of confidence comes from looking at your so called “weaknesses” and realizing they are not. My mind has a steady stream of ideas and turning it off can be a challenge sometimes. But when you can harness those ideas and execute them, that’s when some really amazing things can happen. Reply
Does Stash just make tea? I don’t drink tea, so that’s probably why I haven’t heard of it! And I’m not sure if it’s jello. I plan to have my 4 year-old test it.
Thanks. Yeah, we … Thanks. Yeah, we had one of those at college. I didn’t really like it much. Thought it sounded brittle, but I was comparing it to “professional” equipment. I have no idea how it compares with stuff in that same price range.
hola buen dia, me agrada todo lo concerniente al ramo, me gustaria que me enviaran un modelo para sorpresas del dia del niño para poder ponerles las golosinas y que tenga una utilidad es especificamente solo para niñas de edad escolar nivel primaria. gracias….
Yo! Arthur! you rockTO;ToolTool, you are a tool, you are the tooliest tool that has ever tooled a tool. If I had a wrench and it was the biggest wrench in the world it would still not be as big a tool as you are, you fuckin tool, fuck off and be a big fucking tool somewhere elseYOU TOOL!
If I were a Teenage Mutant Ninja Turtle, now I’d say «Kowabunga, dude!»
If not for your writing this topic could be very convoluted and oblique.
I hate my life but at least this makes it bearable.
Bella arrived in «June»). I want to get us to December 2010, because that’s when Alice gets to join the story, so there’s probably going to be a few instances of «And things went on in that manner for a while» in the next few entries. But the storyline was at a place in 2009 where I couldn’t just be like, «One year later…» So there was some time wonkery I was trying to pull off. Maybe I really should write up a general timeline of when things actually occurred, as opposed to when they were posted.
i think you should pay per visits as in other ads network exists PPC (Pay Per Click) but not per work hour because it depends on human experience.
I just couldn’t depart your site before suggesting that I extremely loved the usual information an individual supply in your visitors? Is gonna be back incessantly in order to check up on new posts
I'd be lying if I didnt say id like to go to update my summmer wardrobe. But I would also like to go for the people watching, I am an avid blog follower,and lets face it parties and London are always worth attending!hbpencil77@hotmail.com
Good to find an expert who knows what he’s talking about!
à ®œà ¯†à ®¯à ®®à ¯‹à ®•à ®©à ¯ à ®Žà ®´à ¯Âà ®¤à ®¿à ®¯à ¯Âà ®³à ¯Âà ®³ à ®¨à ®¾à ®°à ®¾à ®¯à ®£à ®•à ¯Âà ®°à ¯ à ®•à ¯Âà ®²à ®®à ¯Âà ®®à ¯ à ®µà ®šà ®µà ¯ à ®‡à ®£à ¯ˆà ®¯à ®¤à ®³à ®®à ¯Âà ®®à ¯ à ®Žà ®©à ¯Âà ®•à ®¿à ®©à ¯Âà ®± à ®•à ®Ÿà ¯Âà ®Ÿà ¯Âà ®°à ¯ˆà ®¯à ¯ˆ à ®ªà ®Ÿà ®¿à ®¤à ¯Âà ®¤à ¯Âà ®ªà ¯ à ®ªà ®¾à ®°à ¯Âà ®¤à ¯Âà ®¤à ¯‡à ®©à ¯Â. à ®…à ®¤à ®¿à ®²à ¯ à ®¨à ®¾à ®°à ®¾à ®¯à ®£à ®•à ¯Âà ®°à ¯ à ®•à ¯Âà ®°à ¯Âà ®•à ¯Âà ®²à ®¤à ¯Âà ®¤à ®¿à ®©à ¯ à ®µà ®°à ®²à ®¾à ®±à ®¾à ®• à ®…à ®¤à ®©à ¯ à ®®à ®•à ¯Âà ®•à ®³à ¯ à ®¨à ®² à ®šà ¯†à ®¯à ®²à ¯Âà ®•à ®³à ¯ˆ à ®ªà ®Ÿà ¯Âà ®Ÿà ®¿à ®¯à ®²à ®¿à ®Ÿà ¯Âà ®Ÿà ¯ à ®•à ¯‚à ®±à ®¿à ®¯à ®¿à ®°à ¯Âà ®¨à ¯Âà ®¤à ®¾à ®°à ¯ à ®‡à ®¤à ¯ˆà ®ªà ¯ à ®ªà ®±à ¯Âà ®±à ®¿ à ®¤à ®™à ¯Âà ®•à ®³à ¯Âà ®Ÿà ¯ˆà ®¯ à ®•à ®°à ¯Âà ®¤à ¯Âà ®¤à ¯ˆ à ®¤à ¯†à ®°à ®¿à ®¨à ¯Âà ®¤à ¯ à ®•à ¯Šà ®³à ¯Âà ®µà ®¤à ¯ à ®‰à ®¤à ®µà ®¿à ®¯à ®¾à ®• à ®‡à ®°à ¯Âà ®•à ¯Âà ®•à ¯Âà ®®à ¯ à ®Žà ®© à ®¨à ®¿à ®©à ®•à ¯Âà ®•à ®¿à ®±à ¯‡à ®©à ¯Â.
If your articles are always this helpful, «I’ll be back.»
Dec13 I think this is among the most important info for me. And i am glad reading your article. But should remark on few general things, The web site style is great, the articles is really nice : D. Good job, cheers
Great common sense here. Wish I’d thought of that.
ABEL, i must tell you the South-south and South-east most benefitted from GEJ’S govt,though these regions are his political backbone..As a person i like GEJ,but Ogboni frat would not allow him perform.Everything happening in Nigeria today is done by Nigerians(Politician and Masses).My advice to this forum “AS MUCH AS WE BLAME OUR LEADERS FOR BAD LEADERSHIP,LETS CHANGE NIGERIA FROM OUR VARIOUS SPHERE OF CONTACT…..God bless Nigeria
Hi,Same question from my side, uhm it probably is a missing resource compiler – you can get it from . After you’ve put it e.g. into the \\bin directory you must specify its path in the Win32 Resource compiler settings – I know that it sounds awkward but it actually seems that I lastly forgot to mention this point in the installation tutorial :/
You make things so clear. Thanks for taking the time!
I’m impressed you should think of something like that
Yup, that should defo do the trick!
31-10-08òшÿшõ ÿøшõт: ýðрþô þтÿøшøтõÑÂь ÿûø÷ у úðòþ þñрð÷ ýþрüðûьýþ þтúрыÃȄÂÑÂ! ð тþ úðчðть üýþóð уö… Ñыû ûø ÑÂтþт þтòõт ÿþûõ÷ýыü?
Josie – of all songs, that one would have to be a bit of a tear jerker right now with him more than a thousand miles away.I wonder how he’s doing, what he’s doing RIGHT NOW? Whats the time there in Chile right now? When i’ve looked the time differences up in the past there have always been discrepancies.
The success of the treatment is greatly affected by the relationship between the patient and his partner. Acupuncture can correct erectile dysfunction. Self hypnosis can assist erectile dysfunction patients to relax prior to and in the course of intimate moments so that they acquire a stronger grip over your emotions and sexual responses.
Your post has lifted the level of debate
Aren't you surprised lefty bloggers didn't sign on?For example, someone like Jane Hamsher will never vote for Obama, so why would blogger like her decline to sign the petition?
that we should not judge, but it also says “judge all things” which makes it difficult at times, and also confusing. The key here is that there is a difference between judging people’s intentions and their motivation, which is a dangerous thing, and judging their actions which we actually must do because we need to protect ourselves from the wrong influences that so easily sneak in on us. I think that it is important to make this distinction, otherwise we end up accepting anything.
That’s really shrewd! Good to see the logic set out so well.
Asà mismo, los movimientos rebeldes permanecerán en la calles por el momento Demos a conocer nuestro descontento con marchas de repudio a la imposición de la narco-mafiaDESOBEDIENCIA CIVIL ATRAS DEL MIEDO . . . ESTA LA LIBERTAD !!La soberanÃa Nacional radica esencial y originariamente en el pueblo. El pueblo tiene en todo tiempo el inalienable derecho de alterar y modificar la forma de su gobierno
Kym – I’ve been doing project life, digitally, but would love to try it out with real paper. Btw, love all your layouts. I love how you incorporate so much texture and dimension to them.
Thanks for the great info dog I owe you biggity.
You really found a way to make this whole process easier.
But you don’t give that surplus to a group at the expense of another. The CBA was negotiated, now the governor is wanting to violate the contract that was presumably negotiated in good faith.
BS low – rationality high! Really good answer!
Good day! This is my 1st comment here so I just wanted to give a quick shout out and tell you I truly enjoy reading your blog posts. Can you suggest any other blogs/websites/forums that cover the same subjects? Thanks a lot!
hector diyor ki:arkadaşlar bişi sorcam ama lütfen cevaplandırın ben ıphnu turkcell veya vadofonedan almadım. teknosadan aldım. Peki ben bu ıphonu turkcelle götürsem turkcellde dilini türkçe yaptırabiliomuyuz acabaBu yorumu değerlendirin; 0 0
124I am really impressed with your writing skills as well as with the layout on your blog. Is this a paid theme or did you modify it yourself? Either way keep up the excellent quality writing, it’s rare to see a great blog like this one these days..
This article achieved exactly what I wanted it to achieve.
Veto, #155The current owners need to relocate to California…they have every bit of motivation to unload the house quickly (read: low price, and going lower).
a Eastriver: Montilla hablaba catalán antes de ser President. Si estudió catalán fue para perfeccionarlo, por respeto al idioma, cosa que le honra.(Por otra parte su presidencia fue decepcionante desde un punto de vista de izquierdas, pero eso es otra cosa…).Salud.
I really love to come here and read your site and I especially adore this text. I worship your ability to say what you want in a concise form. You at once go to the point and you don’t beat around the bush. I wish that you will continue to write in your style and that you will not change it. Sincerely, Keisha.
Great article, thank you again for writing.
Greenwood Village, CO, had a car drive up the cut down curb [so us old folks don't trip]. The driver thought it was the entrance to a nearby restaurant. She then drove onto an ice-covered pond. The passenger drowned. The solution was a park bench bolted to the sidewalk in front of the pond. OldeForce
That’s an ingenious way of thinking about it.
It’s like a habit of me everyday, to just turn on Ronan on youtube and read your blog. Right till now, the song still makes me cry, regardless of the million times I have listened to it. Persevere, Maya. I know you will never bury Ronan, for he is your monkey, your spicy monkey. He will feel your love. He is feeling your love at every time of the day. Love you, stay strong<3
There’s a secret about your post. ICTYBTIHTKY
.But I would point out that Chinese people, like everyone else, are perfectly entitled to express any views they like here. If they happen to involve supporting the present regime however, then they should expect people to disagree with them. Just like we’d disagree with any Americans who came here supporting Bush (interestingly, I think American New Zealanders are 99.9% Democrat).
You’re a real deep thinker. Thanks for sharing.
Hey There. I found your blog using msn. This is a really well written article. I抣l be sure to bookmark it and come back to read more of your useful info. Thanks for the post. I抣l certainly return.
These pieces really set a standard in the industry.
That’s cleared my thoughts. Thanks for contributing.
Rich, that was the church of my college years. I loved it. I kept tabs on all the charismatic/pentecostal Wheaton students, and an amazing number of us ended up there. After an initial adjustment, I felt very at home.The physicality of the service (standing and kneeling), the centrality of worship, the prayer ministers with annointing oil in hand — it has more in common with the A/G than one would think. In fact, this post has got me so excited I think I’ll just have to post about it on my own blog: Why I Love the Anglicans. Though I haven’t yet sought their ordination.
That’s a sharp way of thinking about it.
They’ve franchised so they’re no longer a one-shot, but MacKenzie River carved out a fairly superior niche of unusual toppings and unexpected combos (and upscale prices) right below in Montana, America.
IMHO you’ve got the right answer!
Thank you Chris. I look forward to my Facebook news feed becoming usable again. One additional point that should probably be made clear is that you have to be logged in to your Facebook account to see the block button.
Extremely helpful article, please write more.
Please stop by and check out our newest giveaway.. Saags Specialty Meats is giving away to Four people who leave comments on the blog post. Thank you for your support,,,..Ashlee.,,.
I literally jumped out of my chair and danced after reading this!
In awe of that answer! Really cool!
I found myself nodding my noggin all the way through.
At last! Someone with the insight to solve the problem!
Heya just wanted to give you a quick heads up and let you know a few of the images aren’t loading correctly. I’m not sure why but I think its a linking issue. I’ve tried it in two different web browsers and both show the same results.
Úgy látszik, nem járok elég nyitott szemmel azon a piacon, mert még sosem láttam Å‘t ott. EgÃnkb©Ã©yt a finn, tágabban skandináv konyhában is közismert, népszerű zöldség.
Great post with lots of important stuff.
Na ultima fotografia do grupo que se preparava para ir a Sonaco,creio não me enganar,mas quem está entre o Tony Levezinho e o Rodrigues sou eu.António Marques
I think that 1, 2 and 4 are Oberon, Titania, and Eden respectively since they’re the first second and fourth most powerful people in faerie, not sure about all of the other stuff though.
Thank God! Someone with brains speaks!
brilliant – as ever! I really love what you've done! You always sewing look easy – maybe I need to drink before I stitch to stop the stress. I love the peasant maxi – perfect for this time of year! xxx
My latest favorite addition to my basic recipe (the above “mom’s go to” link) is millet. And I’ve started using half honey and half maple syrup -best of both worlds!
Its like you research my mind! You seem to find out so much about this, like you wrote the guide in it or something. I think which you can perform with some pics to generate the message home only a little bit, but other than that, that is great blog.
hi Mr Mark,i watched every single of ur episodes and latelyu explain every new tools in cs5 but nevermention 16 bits jpeg .Q is what is the benefit working with 16 bits,saving it and the difference between 8 and 16 bits.Thanks,
Keep these articles coming as they’ve opened many new doors for me.
There’s nothing like the relief of finding what you’re looking for.
va rog bagati filmul cu franco nero pentru un pumn de ceapa western comedie din anul 1976-1978 sau cipolla colt regizor enzog castellari va rog mult este o comedie superba si daca sar putea si descarca filme de pe site ar fii super va multumesc
Well done to think of something like that
ÄŒendo, nechce se mi už stále psát jedno a to samé, takže možná Vás pÅ™esvÄ›dÄà popis reality z jiného zdroje – Liberálnà teorie o hrůznosti pobÃdek a dokonalosti nÃzkých danà jsou krásné, ale skuteÄnost je jiná.
Hyvät kuvat ja suht simppelit reseptit pitää olla että tulee ostetuksi. Usein ystävän tai seuraamani bloggaajan suositus voi vaikuttaa niin että tilaan kirjan netistä siihen sen kummemmin tutustumatta.. Tosin tämän takia keittokirjojeni joukossa on muutamakin josta en ole koskaan vielä edes kokeillut mitään reseptiä!! :)-Irmeli-
Isn’t that the kind of drivel you would expect if a foreign Super Power launched a “TEST” missile off our coast. Heck I bet the Obama White House even made the flight logs reflect that flight. Have they found any survivors of that flight?
Kære alleTak for kommentarerne.Det er så dejligt at få feedback på vore ting. Tak :-)Malin: der kan være stor prisforskel på sifoner. Farve og med/uden skift kan være afgørende. Og alder.Regina: jeg kan se, du fandt kuglerammerne :-)Karina: Du er altid velkommen til at bestille over webbutikken http://www.FROEKEN-ANKER.dkJeg vil ønske alle en dejlig søndag (morgen).Knus Birgitte
Asto file to ti tha ginotane stin ellada to kserome kalla oloi,den iparhun magalitera llamogia apo tous ellines politikous,aytoi den pezoun me xiliades me ekatomiria kai ano,o Tzohatzopoullos to remali ksodepse sto Parisi ena ekatomirio otan ksanapantreytike sta 72 o salemenos geros tou PASOK
Das mit dem Seitenbaum ist wieder klar, da war mal wieder der DAU vorm PC Hab nur noch das Problem das mir die Vorschau im powermail nicht angezeigt wird.Gruß Chris
Hallelujah! I needed this-you’re my savior.
I wanted to spend a minute to thank you for this.
Of the panoply of website I’ve pored over this has the most veracity.
Pelican crossings are very out of fashion with TfL at the moment – it’s still planning on removing a load around London, including the one at the other end of Victoria Way, where it meets Charlton Road.
 ( 2012.02.11 23:31 ) : Your own situation you may capable company the best method to keep here in preparing critical subjects good for web-based corporation. cash
Monet.TedescoI’d have to examine with you here. Which is not one thing I usually do! I take pleasure in reading a post that may make folks think. Additionally, thanks for permitting me to comment!
So true. Honesty and everything recognized.
The forum is a brighter place thanks to your posts. Thanks!
i’d love to see a price to earnings ratio for different parts of the UK. My bet is London massively skews the rest of Britain.- rich, leeds, 01/8/2012 21:47……Not so long ago, house prices down here were nearly 15 times average local income. How does that compare with London or Leeds?
Great Article…I think that is one of the so much vital info for me. And i’m happy studying your article. But wanna commentary on few normal issues, The site style is perfect, the articles is actually nice : D. Good process, cheers!…
Going to put this article to good use now.
Dr. Osmar, uma coisa é certa. TODOS torcerão contra o Corinthians, independentemente do que aconteça no campeonato. Isso só demonstra o nosso gigantismo, somos nós contra o resto. Abraços.
Another issue is that video games are typically serious naturally with the primary focus on knowing things rather than entertainment. Although, there is an entertainment element to keep children engaged, each and every game is usually designed to focus on a specific group of skills or programs, such as instructional math or scientific discipline. Thanks for your write-up.
I actually just responded to Day 15. I’m behind you guys, but instead of trying to rush and catch up, I’m truly enjoying this journey. My comments will be posted about 1 1/2 weeks after you post the new week, but I hope you guys will go back and respond to what I wrote. Reading the Bible every day has truly been a blessing. So, I’ll respond to this posting in about 11 days!!!
I was drawing parallels between Corzine and Christie. It’s amusing to me when a politician, of any flavor, does something stupid and has to spend the following several weeks explaining their actions or “hummana hummana-ing†Ralph Kramden style as the public is asked to accept the dubious propriety of such things as “loans,†etc.
Hey BobbaLou,Jordon looked absolutely gorgeous. Her dress was perfect. I was trying to figure out where I saw the 4 girls pictured with you and then I read the caption. DUH… Mikey, I second your motion the favorite picture.You two take care,Give my grand-dog Murphy a big hug.Momba
Hola quiero regalarle una bateria para wii a mi hijo, que tenga el micrófono y todos los accesorios, alguien me podria dar una idea de adonde comprarlo…gracias
I want XenyTV1 back. Atleast give the account owner a list of reasons as to why it was "taken off". I am quite sure he will inform the rest of Tube if you do so.
Hiya, I’m really glad I’ve found this info. Nowadays bloggers publish only about gossips and internet and this is really irritating. A good website with interesting content, this is what I need. Thanks for keeping this website, I will be visiting it. Do you do newsletters? Cant find it.
its oky not to succead in life know u did wat u could do at the time was enough and have unshackable trust in Creater dat he also has a dream fr u and u will gt it and it will the best dream u coulld dream of or nt dream off or watever u gt wat im sayin i hope………smile)VA:F [1.9.20_1166]
Hi, i think that i noticed you visited my blog so i got here to “go back the desireâ€.I am trying to find issues to improve my website!I suppose its ok to use some of your ideas!!
How neat! Is it really this simple? You make it look easy.
MichaelI think you are absolutely right about the ecosystem metaphor and its emphasis on balance, diversity and dynamism. How about we get a DEMOS/New America Foundation working group, discussion, panel, provocation happening on this – we can hit both coasts, NY and DC? And find some allies in the center of the country and begin to engage in a real discussion about what we need, want and can make happen….Lucy
With all these silly websites, such a great page keeps my internet hope alive.
Trina – Oh, Kelly.My heart just breaks for you and your family. What an awful situation. I have shared your story with friends and family and hope that you are able to get moved and get your basic needs met soon. My family’s prayers are with you.
Today, while I was at work, my cousin stole my iPad and tested to see if it can survive a thirty foot drop, just so she can be a youtube sensation. My apple ipad is now broken and she has 83 views. I know this is completely off topic but I had to share it with someone!
Very true! Makes a change to see someone spell it out like that. 🙂
Got it! Thanks a lot again for helping me out!
Hallo Thorsten ,viele Grüße in den Urlaub aus Deiner alten Heimat Aachen. Vor Jahren hast Du mal gesagt, ein Karriereende in AC könntest Du Dir gut vorstellen. Wir haben jetzt eine blutjunge, exellente Truppe, die einen alten Leitwolf gut gebrauchen könnte. Ruf doch mal Eric an !GrußManfred
I downloaded two videos from Youtube, then KeepVid. I cropped both of the videos on Windows Movie Maker. But the thing is when i put the videos together , the second video seems to pause for a second before started again. When it pauses the music does not pause, it continues to go smoothly. How can i fix this?!?!?!?!?!
haha vänner är sÃ¥ bra <3diggar din inställning i förhÃ¥llande , du o markus er ut att ha ett öppet och kärleksfulls förhÃ¥llande men framförallt att ni har kul .. mitt x o ja hade ej samma humor o det vart skit jobbigt i längden hur dumt det än lÃ¥ter. kram 🙂
I bow down humbly in the presence of such greatness.
Nov13Katharine As someone who has been there and found that the truth of Christianity really is found in traditional Catholicism I can relate . Now the problem has become looking at the Church through the eyes of someone who never really knew God, instead of someone who thought she did.
Most help articles on the web are inaccurate or incoherent. Not this!
DandCVideos, did you not read the blog entry?"We wish we could include everyone, but many countries have different laws about running contests and we weren't able to make a contest with rules that are fair and work the same for everyone around the world."
Grade A stuff. I’m unquestionably in your debt.
It was dark when I woke. This is a ray of sunshine.
19dJust desire to express a person’s posting is often as amazing. A clarity in the posting is definitely just spectacular plus i actually could expect you’re a guru during this matter. Fine with the permission let people to seize a person’s feed to prevent updated by using impending posting. With thanks your , 000, 000 plus i highly recommend you carry on a enjoyable deliver the results.24
C’est à peu près les memes démarches au Québec , surtout le changement d’adresse pour les cartes visa .. c’est important Bon j’espère que vous vous plaisez dans votre nouveau chez-vous Répondre
Cara valentina, grazie per averci ricordato l’aquila, dillinger fara tutto il possibile per mantenere alta l’attenzione nei confronti del territorio abbruzzese
An intelligent point of view, well expressed! Thanks!
Thanks so much for stopping by, everyone :)Gitchie, sounds good!Beth, I can't say if they are better, but for our purposes (raw food), we use kelp noodles because they are raw.Sn, thanks! They are very neutral in taste, in my opinion. Nothing fishy.
The purchases I make are entirely based on these articles.
I just found your perfect_dos_vga_437 DOS font. It seems to be a perfect replica, and I’m so glad to have it now after searching high-and-low for a TTF font that emulates the BIOS-based text-mode font perfectly.Unfortunately, I couldn’t find any information about this font on your web site. It would be really nice to have this. Thanks in advance.Posted by on ·
Yus nous dit le Al Kanz,c’est n’est pas par esprit tribale.. je me questionnais juste sur le pourquoi du commet les musulmans français ne s’étaient pas approprié un marché qui leur revient de droit… Et trouve dommage qu’on doit toujours attendre des autres!
pisze:Panie Arturze,wkradÅ‚ siÄ™ maÅ‚y bÅ‚Ä…d, zdaje siÄ™, nowa festiwalowa idea to „źródÅ‚o zmian” co z pewnoÅ›ciÄ… wiąże siÄ™ też z dobrym smakiem OceÅ„ komentarz 1 0
that subway dude was quite funny… and i got a warm subway ok nothing else to say….. oh yeah answer to Sarah – yes subways are very good they are goooooooooorgeous! try them out and enjoy!
I don’t even know what to say, this made things so much easier!
Great goods from you, man. Teaching the Simple Past Tense and Its Irregular Verbs I have understand your stuff previous to and you are just too fantastic. I really like what you’ve acquired here, certainly like what you’re stating and the way in which you say it. You make it entertaining and you still take care of to keep it smart. I cant wait to read much more from you. This is really a tremendous Teaching the Simple Past Tense and Its Irregular Verbs informations.
dit :Vu comme ça, ça a l’air presque sympa la Nouvelle Star ! Bon, moi, j’arrive pas à regarder cette….J’en profite pour te dire “à dans deux mois”.tchuss….
I thought finding this would be so arduous but it’s a breeze!
“Ah, good ol Colin! For one country, “unqualified loathingâ€, for another unqualified excuses.”If you insist on reading meanings into my posts that simply aren’t there, I can’t stop you — but I fail to see the point.You know, you’re really just a kind of resident troll. You’ve figured out who you can flame and who you can’t — and to what extent — and you just have at it.There’s rarely or never any actual content beyond that. It’s just a disturbed display of hostility towards anyone you feel you can safely attack.
Thank you for another magnificent article. Where else could anybody get that kind of information in such an ideal way of writing? I have a presentation next week, and I’m on the look for such info.
What else can you expect from a corrupted regime?What else can you expect from a people with “get rich qwik” mindset deeply imbued in their brains?
I too love Downtown Disney! We generally schedule some time in our vacation to be able to spend at least half a day here. My kids love Once Upon a Toy and I think they believe it is an attraction in itself! :-)Beth´s last [type] ..
Posts like this brighten up my day. Thanks for taking the time.
Ah Scampi, now you made me feel like a quotes pedant, dammit.But to continue my pedantry, I don’t personally see creating strongly branded commercials as ‘trick’ either.Just good advertising.
Posts like this brighten up my day. Thanks for taking the time.
Hahahaha. I’m not too bright today. Great post!
Great ideas! You can always save some money if you think about it carefully.Also I remember I used to use some packs from Colemans for the casserole mix – you literally just add water and it has the herbs etc in too. I think they were about 40p each or something so not too bad for time saving element!Keep up the good work!
Online dating is … Online dating is basically for having fun. But I can assure that this is a big business and you can find dating websites for any niche you want. Also if you want to start your own site, there are dating scripts for only $350USD. I own a dating website and of course at the beginning nobody wanted to subscribe because there were no profiles in there, so you must create fake profiles to get attention. I dont make good money, Im just making the necessary to live. Was this answer helpful?
Please keep throwing these posts up they help tons.
Felt so hopeless looking for answers to my questions…until now.
E’ stato il convegno più squallido a cui abbia assistito: una gara fra i relatori a chi diceva cose meno interessanti.NWO o non, non me la sono sentita di rientrare in sala dopo la cena. E credo di aver fatto bene. Ne approfitto per salutare tutti quelli che non ho saluattao a cena, e spero di rivederli presto in un’occasione migliore, possibilmente con sraker, che almeno se c’è lui i divertimento è assicurato.
pas dijalankan ad tulisan bgn pak”procedure declaration does not match description of event or procedure having the same name”ini terjadi pada form Tcustomer pada “Private Sub datPrimaryRS_MoveComplete(ByVal adReason As ADODB.EventReasonEnum, ByVal pError As ADODB.Error, adStatus As ADODB.EventStatusEnum, ByVal pRecordset As ADODB.Recordset”
That is a little weird, that he gave you that without knowing exactly what it was…I usually get spots, all over my body, that are slightly whiter than my skin colours, when I’ve been in the sun or when I’m too hot. They take a few weeks to get rid of, BUT cortisone always helps. Maybe you can go get some hydrocortisone and try that? It has “no” side effects And still. You know what you should do about your sad state. I will keep pointing this out to you, until you get it![]
This is exactly what I was looking for. Thanks for writing!
I remember the first time I saw Raiders of the Lost Arc. I was intrigued by Indiana Jones when he managed to escape that first death trap, but then when he admitted to “hating” (read: ‘being afraid of’)snakes, I was totally captivated. If a guy has no chinks in his armor, he doesn’t need anyone–not even the heroine.I so glad you enjoyed TOUCH OF A THIEF! Hope you love the rest of the Touch of Seduction series.
This world cup might not be watchable without ian darke. Not because the play is bad, but because he’s the one real truth-teller. Not afraid to call people out. I mean, Foudy is already projecting a USA-Germany semifinal. Sigh.
For the love of God, keep writing these articles.
As a person with Partial Seizure lumping together the minor and major neurocognitive disorders doesn’t seem like a very good idea. There are to many other neurocognitive disorders besides Dementia and Alzheimer’s Disease to compensate for. Do we get to change our name to?
Your answer shows real intelligence.
This post will be new to many guys because the myth is exercisesare intended for the purpose of body fitness but exercises particularly based for Cardio Vascular organs sounds new to most of us.
Waow , Merci beaucoup pour ces conseils! Désolé aussi je répondre seulement maintenant , Je suis venus voir seulement aujourd’hui , et je suis retombé sur mon commentaire! Un grand merci pour tes conseils , Je vais tester ca! Je t’en dirais des nouvelles!
Oh my goodness… Simplicity brings up such sweet childhood memories. I cut my sewing teeth on patterns made by Simplicity, under the watchful eyes of my Mom and Grandmother. I’ve been eyeing that bias tape maker for some time now… and to the Rotary cutting and Embossing dream machine… very nice to meet you!
A wonderful job. Super helpful information.
If you shop at Tops Markets they have a promo. Not sure what areas of the country this is but if you buy TWO 24 packs you get a coupon for double points & if you buy FOUR 12 packs you get a coupon for triple points plus a bounce back coupon for $1.00 off future purchase of 20 ouncer.I got this from a rep at Coke. Just got off the phone with her.Now I just need to go to the store & see if it is in my area, LOLstay safe,
If you’re looking to buy these articles make it way easier.
Thanks for your thoughts. It’s helped me a lot.
Whoever wrote this, you know how to make a good article.
Hi there, I discovered your web site by means of Google while looking for a related matter, your site got here up, it seems good. I’ve bookmarked it in my google bookmarks.
Deep thinking – adds a new dimension to it all.
Wham bam thank you, ma’am, my questions are answered!
All things considered, this is a first class post
Oh- Yeah. I love those, too. I wish I had the one we had on top of our barn when I was a kid. They are just wonderful old pieces. We bought a copper one of a horse when we visited Maine (similar to the one on the wall) and put it on the garage cupola of the house we lived in at the time. Of course, it stayed with the house….darn it all- xo Diana
No veo la TV por que me pongo de mala leche de lo mala que es. Y sÃ, en este pais solo vas a la carcel si no has robado lo suficiente para parecer respetable. Si es que hasta entre ellos hay enchufados, como en la TV.
I am glad you have two worthy winners and there is some money for now. I know things remain tough but we hope to be able to support you as much as we can.
Yup, that’ll do it. You have my appreciation.
life is more easier … life is more easier now and technology like this I mean marketing through this technology is something beyond any bound. Was this answer helpful?
Hi there! I know this is somewhat off topic but I was wondering which blog platform are you using for this website? I’m getting fed up of WordPress because I’ve had problems with hackers and I’m looking at options for another platform. I would be awesome if you could point me in the direction of a good platform.
How neat! Is it really this simple? You make it look easy.
Mixed blessings with kiddies back to school, innit? On the one hand, they're out of the way for a while (yay!) on the other, rushed mornings, shouty breakfasts, lost books, and the threat of PTA Christmas hell looms.Looking like that though, in a looks-made-to-measure jacket and that wonderful hat, must be a smug feeling? admit it!I just know those girls are going to follow in your stylish footsteps and march to the beat of their own drum. Sod the jeans, you never saw a Victorian slut hanging around in stretch denim, did you?lucy x
Meglepő. Ennyire füstmentes az ICBM? Pedig ez nem is követelmény. Akkor a légiharc és egyéb repülőgépre pakolható rakéták mirét füstölnek még mindig annyira erősen? Fura.Tetszik / Egyetértek: 0 Az értékeléshez be kell
Thinking like that is really amazing
Do you mind if I quote a couple of your posts as long as I provide credit and sources back to yourwebpage? My blog site is in the very same niche as yours and my users would truly benefit from some of the information you provide here.Please let me know if this ok with you. Thanks!
loves to attack "the majority" in the United States and blame them for what is happening. Curiously, though, he is much more lenient on Israelis for what he considers their errors, excusing them by saying "The world's unrelenting hatred has worn them down." "Gary W.," however, cannot tolerate even the slightest criticism of Israelis or comments about Israelis which are anything but glowing, and he tells Auster to stop being so hard on them, saying "I would urge you to cut the Israelis a little slack."
That’s what we’ve all been waiting for! Great posting!
uy! gumamela yan ah…kulay pink…dati madalas kong pitasin sa bakod ang gumamela ginagawa kong pagdagdag sa paggawa ng lobo,yung isawsaw sa tubig tapos iihipan.kaya madalas akong pagalitan ni nanay kasi nakakalbo na ang gumamela samin.
A few good movies? He's a pretty darn good actor these days and most of theones he chooses to do have been pretty awesome.Titanic, Blood Diamond, The Departed, The Aviator…just off the top of myhead.
J’ai lu l’article où mène ton lien. On sent un peu honteux à cette lecture qui dit plein de choses vraies. C’est l’évidence : Federer, aux yeux de ses fans est « sans limites » et on a tous un bon conseil à lui donner pour battre Nadal, Djoko et les autres… On oublie en revanche que l’homme vieillit et qu’il n’a désormais plus de titre à défendre en GC pour les douze mois à venir. On est des enfants gâtés, mal habitués…
You’ve got it in one. Couldn’t have put it better.
The forum is a brighter place thanks to your posts. Thanks!
Oh my GOSH, we love Sunflower Seed butter. Am so happy to know you can get it at Target. WE get ours at Trader Joes. It has a yellow lid there.My son gets it, not because of allergies, but because I agree with you, at least limit the PB until age 3. He HAS had some, with no reactions, but still. AND his pre-school is nut-free, so NONE of the others will work. We have tried the soy stuff, but I don’t like the idea of my kid eating too much soy. (Don’t know about the estrogen link, but still….)
Yup, that should defo do the trick!
There is nothing about this arena that is a good deal. The location is terrible, the financial plan is terrible, the benefit to the city is questionable at best. The whole plan needs to be scrapped and started again from step one.The first thing that needs to be considered is the location. Why build an arena in the middle of downtown when it could be built on the airport lands. It would have direct access to the Yellowhead, the LRT can easily be connected, and the road capacity would fit. Trying to put 30000-50000 people into the arena downtown will snarl traffic for hours.
Thanks Kevin!We all respect that a master never gives away all his secrets and not that I would expect you to (and not saying that you have any either, you know what I mean), just a bit more info if possible would be much appreciated for sure.Anyway, the main thing is you are a real inspiration to us all and countless others. Keep it up man!
This is a neat summary. Thanks for sharing!
At last! Someone with the insight to solve the problem!
TimoHallo, kann die App leider nicht kaufen da laut store leider nicht mehr online. Per suche kann ich die App aber finden. Ist diese bald wieder online?
Thinking like that is really amazing
Ich finde die Auflösung auch etwas zu gross geraten. In meinem Notebook habe ich auch einen HDMI-Out, bisher aber nicht brauchen können.Vor allem für die Internetarbeit wäre wahrscheinlich ein zu grosser Bildschirm etwas problematisch, weil man auch alles anders wahrnimmt(etwa Google Suchergebnisse etc oder die Werbeplatzierung) als Besitzer kleinerer Displays.Ansonsten soll HDMI keine Video-und-Tonverluste zu verzeichnen haben.
Hi Jason.. lol…yup that’s why I specifically didn’t ask for comments, would seem a little ironic wouldn’t it As I was saying in my comments to Sherryl, exposure is definately needed and engaging in comments does build authority and trust. But I’ve seen a few bloggers in recent times, slowly begin shift from writing to “help” their readers to writing to “get a response” which is fine if exposure is your goal…but that doesn’t guarantee you the sale.
It’s like you’re on a mission to save me time and money!
Very great write-up, I am standard website visitor of one? utes web site, maintain inside the great function, also it? utes gonna be a normal website visitor for decades.? The thoughts usually do not really blossom in to fruition until offering indicated your crooks to a new person.? through Tag Twain.
Le conatus du capital, c’est de grossir à partir de lui-même, si possible de manière illimitée.Dilapider le Capital, c’est aller à l’encontre de ce conatus.Voilà pourquoi les riches n’aiment pas l’inflation. Elle ne les ruine pas forcément c’est un manque à gagner insuportable pour eux.
No, it is that stubbornly antibourgeois streak of the intelligentsia, that rains contempt on the soldier, the policemen, the merchant, those ‘bitter clingers’ who do not agree with fundamental transformation, I used to think you understood this,but since you went through the looking glass, absolving the Salafi endorsing the netroots, you lost that
Well I think this goes without saying, but I LOVE THEM, LOVE THEM, LOVE THEM!!!! Thank you so much And thanks for not making me wait to long to see them!!!
I read your posting and was jealous
There is a micro smile when Netanyahu is talking. It is called duping delight . When he sits down he is smiling. His successor on the podium is barely able to hide the grin. But you know, their country is being attacked e.t.c……..
MMMMMM Kitty Roca!Scoop the cat box more often, or put it out of the puppies reach. When I had cats, I kept the litter box in a 1/2 bath and installed a cat door in the bathroom door.Dogs love it because cats don’t fully digest their food, so there’s lots of good stuff leftover in their poop.
Hey, good to find someone who agrees with me. GMTA.
OK, how about this- two of my wisdom teeth haven't erupted yet! Does having half of my wisdom (teeth) make it dangerous?!Soon Anush will have her own teeth in her hand to learn more from.:)
Fell out of bed feeling down. This has brightened my day!
João Paulo Costa:Idéia altamente apoiada! É um baita podcast pra quem ama FA. Ia ser maneirÃssimo ter um com a rodada da semana, até porque a temporada muda muito de semana a semana. Tenho certeza que a maioria da galera apóia a idéia. WHO DAT?
Surprising to think of something like that
don’t do the corset thing, it damages your rib cag and can cause a lot of harm over a period of time of lengthy wearingkickboxing, my sister takes it and she has a really nice hourglass figure
Hi! I know this is kinda off topic but I was wondering if you knew where I could find a captcha plugin for my comment form? I’m using the same blog platform as yours and I’m having problems finding one? Thanks a lot!
other BE coaches? why…only Bobby G was clearly implicated, and for a big time recruit. And he was smiling apparently…Seton Hall should do the right thing and self-report this now that it was published. Somehow I doubt that will happen.
– My wife and i got really fulfilled when Raymond managed to complete his researching using the ideas he acquired through the weblog. It is now and again perplexing to simply continually be handing out tips and hints which often the rest could have been trying to sell. And now we do know we
Perfect answer! That really gets to the heart of it!
We could’ve done with that insight early on.
If time is money you’ve made me a wealthier woman.
GRATULERER sÃ¥ mye med 1. plassen!Jeg var helt rørt da jeg sÃ¥ deg pÃ¥ tv nettopp.Tenk Ã¥ ha Norges Vakreste Hjem ;)FANTASTISK…NYT øyeblikket.Klemmer fra May Helen
A person essentially lend a hand to make significantly posts I’d state. That is the very first time I frequented your web page and so far? I amazed with the analysis you made to create this particular submit extraordinary. Magnificent process!
Action requires knowledge, and now I can act!
I hadn’t read this puppy!!! I love reading your shizzle because it makes me learn how to be a better person and in turn might make people nicer to me!! (See what I did there) But I’m gonna try doing just this – never just a blanket compliment.
Es que si al menos sintieran vergüenza tras hacer semejante alharaca por algo perfectamente natural en un proceso de negociación los lectores inteligentes no sentirÃÂamos tanta indignación, tanta pena ajena. Pero ni eso. Ya me gustarÃÂa verlos por la calle tildando de guerrilleros a todos los politiqueros que hicieron presencia en La Uribe y en El Caguan. Pago por ver ese circo de simios con meningitis.
Shawn thanks for the comment. I too was very independent (still am at times) but when I met Emily I was glad to do life differently; now I can’t imagine life without Emily, and for now I don’t try too. Life is so much more sweet and understandable with her around.
It’s their life and so it’s their right to decide what to do with it. Just like assisted suicide. If they wish to stay in Afghanistan – risking their own life – what the hell right do you have to tell them to do otherwise? Why should fat lazy elitist socialist swine have any right to tell anybody anything? Because they FEEL they know better!
You sure are on a Game of Thrones kick. I still have yet to read this series and still have yet to finish watching all episodes. lol. It’s a good thing you’re reading the books on your Kindle. The books are so thick!Happy Wednesday!!Here’s my
Kick the tires and light the fires, problem officially solved!
Checkboxes! Nice Building up a buffer is smart. If you don’t, you’ll feel like you need to do them on top of evteirhyng else. You don’t need that extra pressure. Good luck with NaNoWriMo!
If only there were more clever people like you!
Always a good job right here. Keep rolling on through.
assalamualaikum???saya batuk lam dahh . pastu sejuk badan tu ad peluh pon ad . ermmm.. batuk saya berkahak dan berterusan . kdg2 berdarah sikit. berad badan tak tturun mendadak .. saya takod ada simptom tb .
Just cause it’s simple doesn’t mean it’s not super helpful.
Det var väl Nicke Pack som släppte den. Fanzinet hette Pack.Nicke har ju senare gjort fanzinet Ettnollett som ju i jultiderna släppte sitt allra sista nummer.Han har en skivbutik i Solna och även en postorder kallad Deliscious Goldfish.Googla!
Absolutely gorgeous suit. What a superb situation at the jumble sale, everything 20p! Mind you, I don't envy you the grannies at the jumble, they're hardcore lol!Shirl x
Would LOVE the above prize pack. The umbrella is just too cute! Another product in your range that I would love is Pram Sun Sail, Sun Shade, I’ve not seen one that stretches to the handle like that. Thank you
Ein kleiner Hinweise:flush_rewrite_rules() sollte nur EINMAL ausgeführt werden und nicht bei jedem, in diesem Fall init Hook, ausgeführt werden. Einmal reicht; ein Besuch der Permalinks Seite bzw erneutes abspeichern der aktuellen Einstellungen hilft auch meistens.
This was so helpful and easy! Do you have any articles on rehab?
Nothing I could say would give you undue credit for this story.
Richard Kind used to go to my gym and I swear to GOD he just fucking stood there. Super creepy. You can see his nose close up from far away.
Paleo Baseline: 14:52 – not super pleased with this, definitely feeling the weekend of travelingDL: 205 (increase by 30#)SP: 75 (increase by 20#)Going to do the BS on Thursday, my legs were dead!Does anyone know if protein (like whey protein) for post-workout shakes is paleo? If not, what’s a good substitute?
Hello there! I just wish to give you a big thumbs up for the exelnlect info you have right here on this post. I am coming back to your site for more soon.
Hi Sandra,How wonderful that you have taken the time to give me such a detailed reply – this is what I needed. You have also helped me to overcome my anxiety which was caused by having used other hydroquonine products previously.I will now follow the exactly the instructions you have given me and will report my progress to you in 8 weeks.Please advise – Do you have a local supplier in Singapore? or do I need to order the new ZO products (Growth Factor Serum, Ommerse & Oclipse directly from US? Thanks so much.Nita
Gefeliciteerd nog met je verjaardag, het zijn wel hele leuke spullen die je besteld hebt. Het boek is echt een aanwinst, ik heb het al -tig keer vast gehad en blijf steeds nieuwe dingen zien, zoo mooi!Geniet van je vrije uurtjes,liefs, Sonja
06/05/2011 – 12:55pmSi fuera un periodista de verdad investigaria, no hablaria de errores arbitrales, siendo un testigo ocular mas en la que otro testigo puede declarar lo contrario. Que averigue si hay ordenes explicitas, ya sea verbales o escritas, que encuentre a testigos de esas ordenes, eso si son pruebas, no sus pareces forofistas.
Wat hebben jullie heerlijk geshopt zeg. Prachtig regaal en die tafel daar zou ik ook zo voor gaan. Gewoon ook de salontafel erbij nemen!Groetjes van Kim
My brother suggested I might like this website. He was entirely right. This post actually made my day. You can not imagine just how much time I had spent for this information! Thanks!
Please teach the rest of these internet hooligans how to write and research!
Apparently the Obama administration didn't get the memo…Venture socialism plods on spurred by junk science: Renewable energy has been held back by cheap natural gas, weak demand for power and lack of political concern over global warming. Efforts to use the earth's heat to generate power, known as geothermal energy, have been further hampered by technical problems and worries that tapping it can cause earthquakes.Even so, the federal government, Google and other investors are interested enough to bet $43 million on the Oregon project.
Right on-this helped me sort things right out.
haha dit :Ouin ben yen a une couple qui ont du sable dans le vagin depuis qu’ils n’ont plus la queue de charest dans le cul…
site…Hiya, I’m really glad I’ve found this info. Nowadays bloggers publish just about gossips and net and this is actually frustrating. A good site with interesting content, that is what I need. Thank you for keeping this site, I will be visiting it. …
That’s way the bestest answer so far!
You have noted very interesting details ! ps decent internet site . “Never take the advice of someone who has not had your kind of trouble.” by Sydney J. Harris.
Your post has moved the debate forward. Thanks for sharing!
You’re a real deep thinker. Thanks for sharing.
Judge Roy Bean would say…”hang’em high, no questions needed, let their own countries pay to ship their rotted corpse back to wherever, or dump them in Arabic Sea with OBL.”
xyah nak salahkan mufti plak… kang kalu dorg ckp berdesing tinge pastu x psal kena banned… yg penting kalu hati mmg xnak berubah, xbleh nak buat hape dah… umrah dah pergi pon tp xde efek jugak..Hot debate. What do you think? 9 1
After we fix the current mess.I think we will colonize space.Americans will always need new frontiers.Free Men are the the alpha,we will continue 2 kick ass .yes we will have setbacks,struggle thru ur wars and rumors of war,but Freedom has Gods Grace.Liberty Valance
Hi Charlene,Thank you so much for contacting us with this question. Yes we still make this wine. If you go into any grocery store or liquor store and request this wine and let them know that Clos LaChance is distributed by Youngs Market, they can order the wine for you.Thank you again for reaching out to us. If you have any additional questions, please email
Thanks for being on point and on target!
Thanks Sophie – I totally don’t get it either why GAPS would make a person so much worse when it doesn’t really seem all THAT different from paleo… it is still a mystery to me!
Until I found this I thought I’d have to spend the day inside.
Can’t wait to meet you!! and yes I so have the little blog feeling []Nicole Reply:February 6th, 2012 at 10:11 pmI look forward to meeting you, Dana…you’re going to have a wonderful time![]
Ja również znam i lubiÄ™ orzeszki bukowe ale nie chce mi siÄ™ nigdy wydÅ‚ubywać wiÄ™kszej ilość.. zastanawiaÅ‚am sie, czy gdyby je podprażyć na suchej patelni i potem dÅ‚ubać – może szÅ‚oby Å‚atwiej? Zazwyczaj wcinamy na spacerze:)Pozdrawiam!
Am 07..02. würde ich zu der Versammlung kommen. Ich habe mit der Gruppe heute auf der Prager Straßegesprochen vielleicht erinnert sich jemand, ich sprach das Verbot in Lüneburg an (über PI) Grüße
Hab es jetzt auch endlich geschafft mein Wichtelgeschenk vorzustellen.(Weiter unten in meinem Post)Auch möchte ich mich nochmal bei dir für die tolle Organisation bedanken!!!Spannend war es auf jeden Fall;-)Lieben Gruß und ein frohes Fest wünscht,Line
yunusDrakensburg Sun Best Chalet Dec 28-4Jan 2Bed 6Slp R17000,Breakers 2 Bed 6 Slp 15-22 Dec R16500Cabana Beach 6 slp 15-22 Dec R16500Margate Sands 8 slp 29-5 Jan R17000Yunus 0845021610 or 0113604176(w) or wapp or BBM29A61AF9 or
People normally pay me for this and you are giving it away!
I precisely necessary to appreciate you once more. I am not positive the points that I may possibly have used without the type of concepts revealed by you regarding this topic matter. It truly was a hard case in my circumstances, however , finding out the expert strategy you handled that took me to jump over joy. I’m just happy for this assistance and then hope that you truly know what an amazing job you’re carrying out educating the rest with the aid of your webpage. I am certain you’ve got never come across any of us.
Hi! I keep my carb intake around 15-20 grams per meal to maintain. I lose on 10 grams per meal. I think this varies greatly for different people. It’s key to figure out your numbers. I think it’s also important to stay the course. The cheat is never worth it. However, that doesn’t mean that you have to feel deprived.Best of luck to you both. Please let me know if I can help.Thanks,Anna
Touchdown! That’s a really cool way of putting it!
Mark my words: we will rue the day we wnt down this path.This is a mistake, and a giveaway of governemtn assets to big corporations.It is a tax hike off the books.Dumb. Incredibly dumb.
Whats up very cool blog!! Man .. Excellent .. Wonderful ..
I will bookmark your site and take the feeds additionally…I’m happy to search
out a lot of useful information here in the put up, we need develop more techniques on this regard, thank you for sharing. http://www.01news.fr/cat%C3%A9gories/a-savoir/
Really trustworthy blog. Please keep updating with great posts like this one. I have booked marked your site and am about to email it to a few friends of mine that I know would enjoy reading..
Tu parles Charles!! je crois que tu fais le plus beau métier du monde! ex aequo avec celui que j’apprends en ce moment! ici quand les choses sont révolues elles « sontaient » aussi dans la bouche de mon 4 ans presque cinq et j’adore ça. tellement que je ne le reprends pas, tu t’en doutes, Elmutt.
Right on-this helped me sort things right out.
Saya kryawan swasta perusahan asing bergrak dibdang otomotif,masa kerja saya sudah jln 7 thn,gji pokok saya Rp.4jt/bln..tpi tmpt tinggal sya mash ngontrak,apakah bisa kredit mobil avanza?,.ditunggu jwaban nya di e mail saya.
I will be putting this dazzling insight to good use in no time.
At last! Someone with the insight to solve the problem!
Now I’m like, well duh! Truly thankful for your help.
Your post captures the issue perfectly!
Full of salient points. Don’t stop believing or writing!
I am totally wowed and prepared to take the next step now.
Congrats on 200 Kim! That's awesome! And what a great giveaway, who doesn't love Sephora!I already follow you on GFC and twitter, but now I'm also following you on Pinterest!Have a fantastic Thursday lady! :)xx Jessica
Bonjour, Je viens de faire l’acquisition du Tablet PC Toshiba Portégé m200 et j’aimerais savoir si le stylet de ma tablette graphique (Wacom Bamboo Fun, qui finira surement entre les mains de quelqu’un d’autre un jour) peut fonctionner sur le m200. Cordialement, Kems
My family is having lots of fun learning the forms in this book. Easy to understand and any child who can read and write can do it. This book helped me interest my children in writing, and sometimes I find them doing it on their own now!
That’s the smart thinking we could all benefit from.
Gillar bilden. Vilken av dem säger jag inte;)PÃ¥ tal om D-vitaminer, tar du nÃ¥gra sÃ¥na? Och det är jättebra med hantlar och stÃ¥ng hemma…om man använder dem…(tänker pÃ¥ de jag har som ligger i garderoben)
I wanted to spend a minute to thank you for this.
Karin: « La discussion devrait tourner autour de ce sujet: Comment lutter contre le trafic de la Vie, de la Personne? »En faisant des lois et en les respectant.
Bill,the “bookmarklet-to-bypass-homepage-vs-reader” workaround is a good idea. But I think you had the right idea originally: google should allow you to decide that option once on the front end through an “account preferences” selection (or something like that).btw, LOVE pukkadita!
An intelligent answer – no BS – which makes a pleasant change
Thanks for sharing. Always good to find a real expert.
What’s Happening i am new to this, I stumbled upon this I’ve found It positively helpful and it has helped me out loads. I hope to contribute & aid other users like its helped me. Great job.
Rhonda – Hysterical! Thanks for the laughs. I almost bust a gut reading your comment!Christine – OMG – that's such a funny story (but not at the time, I'm sure)! I would love to see that picture of you, and I'm looking forward to reading the blog post you write! Jess – Thank you for your enthusiasm. You have a lot of entries in the contest now, so good luck to you and to all the other entrants, too!
I am so glad you found this quilt-along. This process is definitely deepening my experience of the Tao and the I Ching. I don’t think you will be disappointed Taiji. Keep me posted on your progress!
Your article was excellent and erudite.
Your post has moved the debate forward. Thanks for sharing!
4 días-6Los Guns and Roses son la banda más comercial, inútil y mala del siglo, qué asco que me dan por favor. Metallica rock? Al parecer los mexicanos tampoco tienen idea de música
What kind of threat to Israel were Palestinian flags and banners? Or does just being Palestinian mean being a potential WMD? Y’know, demographic time bomb? Can the Witty, who condoned Israel’s violent response, still do so if he dares to watch this, to see the total absence of ‘actual’ violence?
yo creo que deberia ganar taylor lautner es un buen actor, es buena persona y un gran amigo.Es muy mono y musculoso si pudiese conocer aun famoso le escogeria a el
137 Posted by 73 on 11July 10, 2012 at 1b7:39 pm 40 2a7Thank you Sandeep,I did find a house and dog sitter! Everything is falling into place so fast. I am grateful!donnaDonna Merrill recently posted..
Most help articles on the web are inaccurate or incoherent. Not this!
YES YES. We were sitting right behind JJ, it was so cool, he got a huge ovation both nights. (Not as big as Disco’s when he dropped the ceremonial puck, but close.) It was a fix of something approximating what we weren’t getting at Pens games, at that still-locked-out point.
Have you ever considered about including a little bit more than just your articles? I mean, what you say is valuable and everything. Nevertheless think about if you added some great pictures or video clips to give your posts more, “pop”! Your content is excellent but with pics and videos, this website could certainly be one of the best in its field. Awesome blog!
Hey, killer job on that one you guys!
Hello SaudTypically I would try a simple long wire outside to begin with.I think we’ve already discussed the power supply problem that you have in another post.Many thanks, Howard
That’s the thinking of a creative mind
Newspapers aren’t licensed, but they should be, just as commercial radio and television stations are. The second step is to enforce standards, so that opinion is not reported as fact.What next Mr Denmore – licensing websites, blogs and twitter feeds?
Wow! Talk about a posting knocking my socks off!
I read your post and wished I was good enough to write it
I searched a bunch of sites and this was the best.
Do you have them all Fantomas?I have Who Cares a Lot, the new one and have just ordered The Works.Are the others worth getting at all, in your opinion?
A minute saved is a minute earned, and this saved hours!
Amazeballs! I went to the "mall" with one of my friends today, and there were so many overpriced dresses in exactly this style. Except, yours is an incredible amount nicer! Love the green & the cut is marvelous on you!
How was I going to break this old habit which was reborn during the holiday season? The answer seemed obvious. I needed to crack down on our spending and use what we have already stockpiled. So, I am joining the Good Cheap Eats Pantry Challenge.
In the complicated world we live in, it’s good to find simple solutions.
Good job making it appear easy.
A really good answer, full of rationality!
A lucid postulation of a general systems theory of energy, psychology and the mind.In a pragmatic technological teaching manner, Swamiji connects us to our psychoenergetic mechanism through a direct transmission and activation of this primitive Life Force Energy. Our gratitude and love for Swamiji is embodied in this boundlesss energy.(Dr) John Twomey,Cambridge College,Tufts Univerity School od Medicine.
Five lemons? Perfect! I've rarely met a poundcake that I didn't like–or anything with lemons to flavor. It is the one cake that I don't mind "falling"–creating some denser areas. My sisters and I learned this from our grandmother–except she meant for us not to jump around and cause the cake to fall. We reversed that "recipe". I'm pushing "print".Best,Bonnie
Thanks for the sensible critique. Me & my neighbor were just preparing to do a little research about this. We got a grab a book from our local library but I think I learned more clear from this post. I’m very glad to see such great information being shared freely out there.
Steve, let's be clear: the so-called black overclass is principally composed of sub-115 IQ welfare-grubbing punks like Obama and Gates.Both Obama and Gates are the beneficiaries of academic welfare–thus their "class advantage." Bottom line, neither is talented or necessary.Polanski
Ok I tried the exercise you recommended in the first video at about 1 PM today and now its 5:50 PM and my pain is no longer there!! Usually when I am done driving around (to pick my mom/dad & sister from work) the pain returns but its not there at the moment!! I am so relived! I will make it a part of my daily routine and see if this goes away for good!! Thanks for providing such effecting techniques/videos
I don’t own two HD 7870′s or one. I own one HD 7850 that I have overclocked to HD 7950 or GTX 580 performance levels. I am perfectly satisfied with my CPU. It’s more than good enough for gaming. While overclocking my HD 7850 and seeing other people’s results. I realized a lot of the them had i5 2500k’s running at 4.0ghz+ and i7′s. With the SAME exact stock speeds as my HD 7850 and my i5 3450, the benchmark results were within a margin of error. Meaning it was at most a 1 FPS difference,
This insight’s just the way to kick life into this debate.
If time is money you’ve made me a wealthier woman.
Das ist keine gute Idee, ich komme nun seit 10 Jahren mit Gruppen nach Herrenwies. Aber wir kommen nur falls es die Bedingungen erlauben und wir uns vorher informiert haben ob die Loipen und die Hundeloipe fahrbar sind, was bisher auch sehr gut funktioniert hat und nun sollen wir für diese Information vorab bezahlen? Das passt nicht in diese Zeit der Apps usw. Wir fahren dann weiter bis zum Kniebis….
Impressive brain power at work! Great answer!
It’s about time someone wrote about this.
Thank you for every other wonderful post. Where else could anyone get that type of info in such an ideal approach of writing? I’ve a presentation subsequent week, and I am at the look for such information.
I think deep down the Israelis know that Gaza is going to bring the whole thing down. They can’t exit the status quo because they know that nothing including Gaza called a state is remotely sustainable.
términos a través de los cuales llegan los visitantes a este artÃculo:pisos compartidos suiza pisos compartidos suiza piso compartido pisos compartir en suiza 2012 foro pisos compartidos suiza piso compartido en suiza normas de pisos compartidos normas de convivencia en suiza pisos compartidos en suiza gente suiza
Can Google please provide me a way to block any sites using FCF from my search results? Nothing annoys me more than clicking through to some site to see some content, and then getting hit with a paywall when trying to explore that site further. I'd rather Google simply not show me these sites at all, as if they're going to restrict their content using such a policy, I'd prefer not to give them any of my business.
How neat! Is it really this simple? You make it look easy.
Gosh, I wish I would have had that information earlier!
That’s an inventive answer to an interesting question
Life is short, and this article saved valuable time on this Earth.
VÃte, panà vážená psycholožko, v luzÃch Äeských když zaznà slovo test, tak půlka kantorstva vidà rudÄ›… ChtÄ›lo by to osvÄ›tu, že nenà test jako test a ne každý je znalostnÃ. Ale zase si Å™Ãkám – kdo nechce vidÄ›t, ten stejnÄ› neuvidÃ.DÄ›kujeme za zajÃmavé pouÄenà ze svÄ›ta nám mÃrnÄ› skrytého duÅ¡ezpytného a pÅ™ejeme JežÃÅ¡ka, aby Vás potěšil. Fakt. Hezký veÄer.
Conocimiento Colectivo; Ser Universal…Ninguna verdad es absoluta, seguramente ya habran escuchado ésta frase, por lo tanto este post no representa nada nuevo de lo que en verdad intuyen. Sin embargo, puede que algunos no quieran ver más allá de su propia idiosincrasia y por tanto, sientan …
I truly enjoy looking at on this web site, it has got wonderful posts. “One should die proudly when it is no longer possible to live proudly.” by Friedrich Wilhelm Nietzsche.
Colons!~ I think the problem with any advice coming from anyone here is that… well they went from here. Which is decidely more common and simpler. Lemme see what I can dig up. There's bound to be something cheaper than $2000. If I can get home and back for $1200, there's no reason you should be paying that much. No chickens in the hotel room, please. Whatever you and Kevin Smith do on the flight is between you two, but I don't want livestock in my bed. This time.
You’ve managed a first class post
Cindy, I am so excited I can’t stand it. I literally stumbled onto your sites by using bing. I have been making paper beads and have been looking for info that way. One of your videos that I watched was the watercolor/clay technique. I just had to tell you the round one, if in blues and greens instead of the pinks could have been the globe. That process has made me decide that this is something I want to do. Thank you so much!
Hi! Thanks for sharing your video. This will definitely help people especially with medical issues in deciding whether to have braces or invisalign. You have a great blog here. Keep it up! Will definitely watch out for your next video.
I can’t hear anything over the sound of how awesome this article is.
Det var ogsÃ¥ meningen at jeg ville spare op, men jeg kan bare ikke vente… sÃ¥ jeg gÃ¥r pÃ¥ kompromis, og køber et EOS 1000D, som koster under 3000,- Jeg ville ellers have haft et 500D, men det koster over 4500… Men mit gamle IXUS er ved at være klar til pension, sÃ¥ jeg kan ikke vente længere…
NÃO CALHORDA PETRALHA. Os métodos que usaram para beneficio de a TODA a quadrilha,independente de facção dentro do pt, foram os mais sujos e sórdidos jamais visto nos quinhentos anos de história "deztepaÃz". O "mea culpa" depois que tudo foi descoberto tem a mesma analogia dos ratos fugindo do navio que está afundando.
Surprising to think of something like that
Ah, i see. Well that’s not too tricky at all!»
i like how all videos say blottes and stuff can be purchased at your local homebrew shop , seriously i lived in ATL and Charl. NC, bot major cities and havent found anything remotely close to thess so called homebrew shop
you can die for your convictions without taking out others with you. he held innocent people hostage with enough propane to kill lots of them. is this ok?i guess i'm not getting why this lunatic isn't getting condemnation for what he did. he's no martyr to the cause of environmentalism.
If polling data tends to show that women are more likely to report belief in things like miracles and astrology, what are we supposed to do about that preconception? I know that in my own dating life the women who DON’T mention astrology are few and far between, and that’s AFTER I’ve selected them for brains and nerdiness. Granted, the dudes in my life are statistically more likely to believe in UFOs or government conspiracies, but I tend not to date them.
Could you write about Physics so I can pass Science class?
The Dietes would sort of echo the shape. The tall Cyperus you have growing IN the pond will also grow planted in the garden, and would take the shade. Try it? Tongue in cheek, a matched pair like the left and right hand. I’m amused that THEY say you must plant matching pairs, but they can’t do what you pay them to ;~)
Real brain power on display. Thanks for that answer!
I think photogrphy like this is very neat, im not always into stuff thats “dark” but i think photos like these are very creative. Ive always had in interest in photos that are kind of strange. Cant wait to see what you come up with ! -Travis Gess
I know this when off topic but I’m looking into commencing my own weblog and also was wondering what just about all is needed to get create? I’m assuming a blog like your own would cost a pretty much? I’m not very net smart so I am not 100% positive. Any suggestions or advice could be greatly appreciated. Cheers
És jó dolog, hogy te voltál 5 éven át a vezetÅ‘nk: új iskola, új óvoda, DumaszÃnház, új művelÅ‘dési ház, új programok, országos turizmus. Visszavárunk!
A little rationality lifts the quality of the debate here. Thanks for contributing!
I’m impressed. You’ve really raised the bar with that.
Wow! Great to find a post with such a clear message!
Felt so hopeless looking for answers to my questions…until now.
commodore staff21/11/2012petite question, ayant une carte bleu a debit differe vais je devoir payer mes depenses de decembre 2012 au mois de janvier 2013 malgre tout?
why oh why oh why… are you crazy!! you have lost me as a youtube site visitor because of the view count feature being removed.!! bring it back!!! who's bright spark idea was that.. not very smart!
Perfect shot! Thanks for your post!
Your posting really straightened me out. Thanks!
wow sophie you had a REALLY interesting childhood! thank you for sharing with us everything with photos & all! i think you're a open & down-to-earth person.. all the best for your future!
Hinata Coucou, bref voilà je suis nouvelle dans mon bahut…..et voilà il y a un gars qui me plaît beaucoup le seule problème c’est que je suis timide et lui aussi sauf que lui il a un sérieux problème, il croit que les filles sont sources d’ennui , je le comprends, il a 3 sÅ“urs et moi j’ai 3 frères et je le comprends un peu sa position, mais comment faire pour le draguer ? 0 0
comentou em 11 de julho de 2012 às 14:43. Te amo ainda mais Jana!!! Normal girls é o que há! Afinal elas são maioria no Brasil… Elas ditam mto mais moda do que as ditas ‘it’… Elas comprar, elas que fazem a economia do paÃÂs girar… Elas que saem loucas em promoções pra gastar seu suado $$.. Parabéns a todas as normais girls que exitem por ai… =D
diyor ki:Bu resimlerden bende yapıyoruuuum. Ben kalbin yanınabide dudak resmi çiziyordum. Kızlar anne bu ne dedi. Bende dudaaak dedim Yani anlamı ne dedi birisi. Sen okulda olsanda kalbim hep seninle ve seni kocaman öpüyorum demek dedim bayıldılar GD Star Ratingloading…
For the love of God, keep writing these articles.
Its still surprises me, how lots of people have no idea about Kinovelax Diet Plan (google it), although many people get great result because of it. Thanks to my work buddy who told me about Kinovelax Diet Plan, I have lost plenty of weight by using it without starving myself.
Thanks Donald. Out migrant tradesmen you have to admire. Apart from making money they will ensure that people get good skilled work done on their homes. All good stuff for the economy.Bob
Nydelige inspirasjonsbilder! Dåååån!Jeg gÃ¥r nok for lilla valører i Ã¥r og, kniiis, kombinert med beige-brune nyanser og en dæsj grÃ¥tt! Det mååå jo bare bli bra det! ;)Fiiin dag til deg søte!Klem fra meg ♥
Hi Heather!!Loove this collection thank you so much for this chance to win. I live in Barcelona so we don't have Joann's here, and you can't imagine how much I like this collection.I'm a follower too.Thanks for sharing those beauties with us 🙂
Hey Cassey! I just like to say that I (mentally) love you workouts. It’ll be a while before my body agrees though. Anyway, I don’t have the time or the financial ability to follow the diet plan that you laid out so are there other plans that can help me eat healthier but are cheaper and much easier to fit in a busy schedule?
Why are you guys talking about extracting wealth from imperial holdings. Isn't the hot lead standard partly about the fact that we can't be conquered? Image if back in 1938 you had payed US dollars, or aussie dollars, for polish money of british pounds. What happened to those currencies? Were they toast?
I had been honored to obtain a call from a friend as he located the important guidelines shared on the website. Browsing your blog post is really a real great experience. Thanks once more for thinking of readers like me, and I hope for you the top of achievements as being a professional discipline.
It’s spooky how clever some ppl are. Thanks!
Dear Sir,Is surcharge payable by a company having income of less than one crore on Dividend distribution tax and if so under which section / provision of the Income Tax Act ?Thanks.
Well, ESXi is now free, right? So, the replacement is ESXi in reality. If you need to run it on Windows or Linux, there is the (non-free) Workstation product that now offers most of the features VMware Server had.
Now I’m like, well duh! Truly thankful for your help.
yourself studying does not help much on the SAT. That’s why when UCAL abolished affirmative action (which affected whites and Asians equally) and instead changed its weighing of SAT and gpa, Asian representation shot up relative to whites.
A simple and intelligent point, well made. Thanks!
Thanks Christine for reminding me what I started reading when I finished with ‘children’s books’ – crime stories, particularly anthologies of short crime novels, which then developed into thrillers and horror books (King and Koontz) and from then into SciFi, which I haven’t escaped from, although I do read the odd ‘other’ book, such as a certain author’s first novel Sorry Lindsay for going slightly off tangent, although you did ask if we had read the same books.
Your posting lays bare the truth
I agree with Joe. Stop ruining franchises Kinect. A better motion gaming is the Playstation Move or the Wii. Even the first motion controlled games are better then anything kinect can do. Or my name for kinect Can’tkinect
support is as vital as well. Children who are encouraged by their parents and are provided with the right support normally perform well in what they do. It inspires them to learn more when they know their parents
I think authority sites are the only way to go in affiliate marketing. Cheesy fake review sites are useless when doing due diligence on a product you might buy. I also check WSOs on the Warrior Forum before buying anything. Warriors are authorities all their own and can save you a fortune.
Flipao, no se trata de ir con todo el morro. Pero entenderás que en el dÃa a dÃa vemos constantemente como mucha gente piensa que todos los servicios del sindicato deben estar a su disposición gratuitamente. Incluso cuando no está afiliado.Por supuesto que no conozco tu caso ni los detalles del mismo. Y, como te dice Jose, lo mismo el compañero te aconsejó muy o muy mal. Pero entenderás que, más allá de ese caso, el sindicato trabaja en muchos aspectos.Pd: “camaradas” son los comunistas, yo prefiero compañero
I’m sharing my French Lentil and Vegetable Soup, one of our favorite Quick and Easy dinners, and my new weekly feature Menu Inspirations. Thanks for hosting and have a great weekend!
That kind of thinking shows you’re on top of your game
For the love of God, keep writing these articles.
Hello! My wife and I live in Phuket, where we homeschool our daughter. I would LOVE to be a contributor on your site. I am passionate about parenting, childbirth, and alternative medicine and we hope our next child will be born VBAC either here in Phuket or in Bangkok.
Do you know that Christianity is correct? The world around us reveals that G-d DOES exist, and the historical evidence reveals that Jesus Christ really did come to this earth and there is overwhelming evidence that Jesus Christ really did physically rise from the dead. Jesus is coming again and the signs of the end times that were foretold in the Bible are coming to pass.
Nice angle for the presentation. Weird that no one has unpacked the why on their blog. Of course I don’t read the everything, so… nothing new under the sun. But then you know that old managemen axiomt: repetition is key. It’s true.
Thanks for taking the time to post. It’s lifted the level of debate
Sou da opinião de que Nelsinho merece uma 2a chance. Acho que os dois dariam certo como companheiros de equipe.Seria incrÃvel para a F1 esses sobrenomes juntos.Se eu fosse a Telefónica ou um concorrente do Santander (Ferrari), corria atrás da equipe para viabilizar tudo. Da mesma forma a Petrobrás.Mas acho que Ecclestone está sonhando com isso e dando um jeito de viabilizar isso tudo.
Hey, killer job on that one you guys!
Dear Steven: You tipped me to nothing. I was on this story 2 years ago before it went public. I did not cover it because I’ve been on the road and it’s been difficult to get online. But I’m not your f*****g errand boy you don’t tell me what I should cover.
At last, someone who comes to the heart of it all
For the love of God, keep writing these articles.
My favorite smoothie combo is the Chocolate Cherry bomb combo (haven’t seen you make it in a while!) – chocolate protein powder, frozen cherries, banana, water/coconut milk and whatever else I feel like mixing in.
You’ve made some persuasive points in your article that are very thought-provoking. Your material is so persuasive that you have changed my mind on many points in your article. That’s how you know it’s good.
caWow, amazing blog layout! How long have you been blogging for? you make blogging look easy. The overall look of your site is excellent, let alone the content!
coucou admiratif pour la patience à tout expliquer avec autant de soin et images à l'appui….pour la gentillesse à se donner tant de mal pour aider et faire plaisir…pour tous les partages d'idées….pour tout le travail que tout ça représente!!!Bravo aussi pour tes réas bien entendu toujours si "travaillées" Bonne continuation et encore Merci pour toutBisesMC
Holy concise data batman. Lol!
Please teach the rest of these internet hooligans how to write and research!
Okay I’m convinced. Let’s put it to action.
MouNziRa dit :qu’est ce que le gabonais lambda peut faire face àla situation, comme si elle avait les moyen de se débarrasser de ces ordures…C’est àla mairie de viabiliser une 2e decharge mais bon sa il devais le prévoir depuis kala, làon voit bien qu’ils sont pris au dépourvu, bah maintenant il va falloir casquer…
Just do me a favor and keep writing such trenchant analyses, OK?
That’s an expert answer to an interesting question
Jonerzz – thanks for sharing. Goofy smile indeed. Like, yes! yes! yes! LOLEven from afar, he brings joy (niff, sniff)Dang! That kid better be ready for major archu-lovin’ when he gets back. Sometimes. when I think about it… I get scared for him, ahahahahahahahahahahaHAPPY HOLIDAYS SNOWANGELZZ!!!
What an awesome way to explain this-now I know everything!
You guys are evolving the internet! Thanks, you make my business sooo much easier. I am a performer and now when people want to see some demo clips, theres a universal format… YOUTUBE! Does the word Youtubular exist yet?
This is very interesting, You’re a very skilled blogger. I have joined your rss feed and look forward to seeking more of your magnificent post. Also, I’ve shared your web site in my social networks!
Knocked my socks off with knowledge!
Qué maravilla de sitio!! ciertamente, el paraÃso de muchos fotógrafos y aficionados *_____*Dani Santi, más q por comparación muchas veces es por desconocimiento de este tipo de sitios por estas tierras españolas nuestras… gracias por la info
Almost all of the things you say happens to be supprisingly precise and that makes me ponder the reason why I hadn’t looked at this in this light before. This article really did turn the light on for me personally as far as this specific subject goes. Nonetheless at this time there is actually one position I am not too comfortable with so whilst I make an effort to reconcile that with the actual core theme of your issue, allow me see what all the rest of the visitors have to say.Well done.
C’est n’importe quoi… Faut les avoir bien accrochées pour réclamer ça..Sinon, bien la photo (même si Dwight n’est pas le genre de type à jouer pendant les heures de bureau )
Funny to see the comment by Joe Grant. I was going to ask if you've been hanging out with him: the pics (especially the B&W, very artsy!) remind me of the great posts Joe does.I share them under the heading "Trail-running Porn". 🙂
I’m not from England, but like following this blog. Can anyone explain what the irony is, about that Tesco ad and the pease being flown in from Guatemala? I think it is tremendous ad, the text, the looks, everything…Thanks.
Yours is a clever way of thinking about it.
Charles I agree. Lexie doesn’t belong in a jail but in a mental facility that can give her the help she needs. I would suggest writing Judge John “Jay” Hurley and Lexie’s public defenders;voicing your concerns.The only information that I have gotten so far is she is in the North Broward Bureau jail (1550 NW 30th AvenuePompano Beach, FL 33069 Arrest Number: 571206647 ) in the 12MW (Female Infirmary).I will keep you updated as soon as I hear more.Mary Pat
"It is astonishing to me how much Obama looks like Malcolm X."More like Frank Marshall Davis. He also looks like Stanley Ann and Stanley Armour. No resemblance to the Kenyan, but then people (whites) aren't used to looking for family resemblances among blacks and mulattos. Any feature that departs from negroid type is simply attributed to white ancestry.
I really appreciate this post. I’ve been looking everywhere for this! Thank goodness I found it on Bing. You have made my day! Thank you again! “Every time we remember to say thank you, we experience nothing less than heaven on earth.” by Sarah Ban Breathnach.
Thanks for sharing the really outstanding support you’ve gotten from the Premise support team, LaVonne. I know I was really impressed when I heard about how much work they did to help you make sure that your project could go live!– Kathleen
Lucy–Thanks very much for the shoutout–and also wanted to mention that we’re going to be launching a GlobalGiving Green site very soon. We think of it as the intersection between international development/philanthropy and climate change–how to continue to support communities in the developing world prosper in a carbon-smart way …
A provocative insight! Just what we need!
Finding this post. It’s just a big piece of luck for me.
Thank you! I power-tested this over three days to be quick with a review, since I had the good fortune to find it so early after its launch.I hope you are not right with your idea that this is the last of the series, but you very well might be true, the return on home turf, what can follow that?You are in the draw of course, Australia is just as far from me as everything else.
Francisco, I got your idea but don’t you think that users are already reluctant with the registration process will prefer an additional step here. But it will be of great help where the security is of importance and your method can really be helpful for social media companies for sure.
in the late 1850′s and has been in private hands until it went public in the 2008 IPO. The MEXICAN STOCK EXCHANGE BOLSA MEXICANA DE VALORES handles, federal securities (bonds and cetes), government development, investment unit, and
Surprising to think of something like that
in the first place, and directly responsible for my success within it having introduced me to Robert Kennedy who would later become my mentor. I love her to death and hope the pics do her justice. #gallery-1 { margin: auto; } #gallery-1
hmm, Mystes – well, yes and no. i lived in abq. too many times, it was a second/third home, and until this year i visited every summer. reminds me of a little LA now. i’ve always attracted the young’uns, and the one person i ever felt the most connected with was 9 years older. so i’m down with the UP, just haven’t found the right UP to get true-ly down with me. thank you dear Ms. M, i do appreciate the foci and reminder that even tho i live in the city of lost causes, i may not be. ♥☮♫
Känner att det är dags att jag läser något av Funke, har hört mycket om henne de senaste veckorna.Ska nog börja med Bläckhjärta.
Velma was one of the sweetest, kindest most thoughtful people we have ever known. She also had a very good sense of humor. She always treatened to pinch Frank and Wade for not being quite enough in church. She will be missed by lots of friends!!
With this advantage, rimless eyeglasses are suitable for everyone. Being popular in the 50s, those rimless spectacles are now on the runways. Currently, rimless glasses are available in some heavyweight names, including Prada, Gucci and Louis.
My brother suggested I might like this website.He was entirely right. This post truly made my day.You can not imagine just how much time I had spent for this info! Thanks!Best Regards Justin Elio
I am curious to find out what blog platform you are working with? I’m having some minor security issues with my latest website and I would like to find something more safeguarded. Do you have any suggestions?
I was just doing some surfing on my Google Phone during my lunch at work , and I happened across something I thought was interesting . It linked to your site so I came over. I can’t really find the relevance between your site and the one I came from, but your site good none the less .
Commander Propecia [url=http://propecia.e-monsite.com/]propecia.e-monsite.com[/url] sans ordonance
Heya i am for the first time here. I found this board and I find It truly useful & it helped me out much.
I hope to give something back and aid others like you aided me.
Keep on writing, great job!
Porém calma, não estou falando de aumentar os
peitos em 8 números, como aquelas siliconadas que
aparecem na televisão.
Perfect Biotics by Probiotic America – Does it Work or Scam?
Perfect Biotics by Probiotic America Review: Probiotics are some of the most popular health supplements these days and for
good reason. They’re harmless enough to be offered to children without any concern but can prevent or treat a
variety of health problems. They’re the «good» bacteria that we’re
all eager to ingest simply because we know it benefits us,
but not many of us stop to think what really is found inside a specific
supplement.
We think they’re all good, and both supplement and food industry take
advantage of our willingness to give many different brands
a try. That’s why probiotics are now included in foods that
make them very much useless, and things are not much different
when it comes to supplements. Low-quality products will include bacteria that is
only alive at the time of the packaging or blended with substances that will cancel it’s expected benefits.
And a particular kind of supplements that consumers must be especially careful with are those that are only available through the internet,
because while some of them are quality products, most are just
part of money making schemes that only benefit the manufacturers.
What is Perfect Biotics by Probiotic America?
Perfect Biotics product is one of the probiotic supplements that is
not available in stores, and it’s manufactured by Probiotic America,
a fairly new company. Right from the start we know that we can’t
have a look at this product without purchasing it first, which is a trait
of internet shopping that many companies are willing to take advantage of
by releasing useless or dangerous products. But that might not be
the case with Perfect Biotics, for which the company
gives much useful information on the official website.
Actually, the website presents all the products manufactured by Probiotic America, and by this feature alone the company
gets some points in its favor when compared to other businesses that
market their products through the internet. First, they offer more
than one product, which means that the company wasn’t founded just to promote one money making product as a result of a new fad.
And second, all products can be found in a single place, which means that Probiotic America is
not afraid that one of them might discredit their name. Often times companies will create different websites
for each product just so the others won’t be avoided when one of them inevitably proves as ineffective (or even worse, causes health damage), but in this case,
it seems like no such concerns exist and the company
stands behind all their supplements.
Perfect Biotics is their first release, and it’s claimed to be a simple yet very efficient
probiotic. It contains 15 species of bacteria and no other substances,
as it’s designed to only do exactly what a probiotic should,
which is helping the digestive system by fixing health problems caused by an insufficient amount of bacteria while
at the same time promoting a healthier immune system.
The CFU (colony forming unit) count is very high, with users ingesting over 30 billion live organisms from one single capsule.
This is also a very good feature of the product, with higher amounts of bacteria being naturally more effective, but the truth
is that each consumer will need a specific number of probiotics depending on their health requirements, and
such a high number might not be particularly helpful.
Still, the results should be noticeable much faster with a high CFU
count, and in the case of Perfect Biotics the company
claims that the effects will start to manifest in around 3-4 weeks of use in most cases.
It’s also mentioned that with some users have experienced positive changes in just a few days, which is very normal for a
quality probiotic.
Does Perfect Biotics Really Work?
No customer opinions are yet available for this product,
but judging by its qualities the users should have some very high expectations.
Perfect Biotics contains some of the healthiest bacteria strains known at the moment,
and on top of that in very high amounts. This means that it should be able to help even those with very
bothering health issues, even though it’s not actually a
medical treatment. Probiotics are classified as foods by the FDA,
as they’re not required to evaluate them because they’re not potent enough to
pose a danger to health, like medication, usually is.
So is the case with this product, which is only supervised and approved
by a doctor who is specialized in family medicine and practices in California.
It doesn’t seem like one specialist could
help much, but most internet supplements give no information about the manufacturers,
never mind the professionals involved, most often because there are none.
But the products offered by Probiotic America do come with some backing, and
they also have the advantage of being manufactured in the US, a trait that
is usually very appreciated by the customers.
It’s claimed that the bacteria cultures are raised in Wisconsin, tested and packed in Utah
and shipped from California, where the company is
also based. The official website also states that Perfect Biotics is tested by third party laboratories, but it
doesn’t offer any proof even if it seems like some documents were supposed to be available for viewing.
Maybe they’ve been removed or the website encountered some errors in displaying them, but either way we have
no way of knowing if the statement is actually
true, at least for the moment. Still, the label of the supplement bottle is
posted on the website and offers all the necessary information. All the ingredients are disclosed,
and we know exactly what species of bacteria are included.
This is very important, as specialists advise against products
that don’t mention the bacteria strains, the
CFU count and the total quantity of product found
in the capsules.
And the capsule packing is also an advantage,
with this form being the most beneficial for the live
organisms and of course for the health of the individuals that ingests
them. The bacteria has to make it to the colon, where most of its amount is supposed
to be and where it’s the most effective. Also, Perfect Biotics is flash frozen before packing, which means that the product won’t have to be refrigerated for preserving the bacteria and
can be kept at room temperature even for years without losing its properties.
The probiotics will stay alive for a very long time, a mandatory trait that is not commonly verified by customers before purchasing this kind
of supplements. Many companies will sell dead bacteria to non-informed clients, with their defense being
simply the fact that the product does indeed contain probiotics.
What Are the Ingredients in Perfect Biotics?
As we’ve mentioned before, the website does a good job
at presenting all the important information about the product.
Perfect Biotics supposedly doesn’t contain, gluten, soy, lactose or any
other allergen source, although nothing is mentioned about any GMOs
(genetically modified organisms) being included.
Quality probiotics shouldn’t contain this type of ingredients, and hopefully, this one doesn’t either, but on the other hand we do know what the fillers are, and they don’t include sugar (commonly used in cheap
probiotics) or other substances that will decrease the qualities of the
bacteria. These are rice maltodextrin, anhydrous dextrose, vegetable cellulose and stearic acid, and none of them are
supposed to harm the bacteria, but nothing
is mentioned about the product being vegetal so we can assume that the capsule
shells are of animal origin, like in the case of many other supplements.
Given that probiotics contain live bacteria, it would seem like they’re
by default unfit for vegetarians and vegans, but as we naturally carry them anyway, the only problem might be their origin. And in this case, we have no
idea what that is, and it would be mentioned it were vegetal, but most likely they have been produced
with aids of animal origin, so we wouldn’t recommend Perfect Biotics for vegetarians.
The bacterial strains included in this product are:
9 species of Lactobacillus (acidophilus, plantarum, rhamnosus,
casei, salivarius, bulgaricus, paracasei and brevis)
5 species of Bifidobacterium (lactis, breve, bifidum, longum and infantis)
one species of Streptococcus, which is theromophilus. This last
probiotic has a name that makes it sound extremely unappetizing, but
it’s actually very beneficial for digestion. It helps the
body digest milk, and at the same time has antibiotic effects that will protect
the organism from infections. This seems rather unusual given that antibiotics are known to kill
probiotics, and it’s recommended to always use this good bacteria along antibiotics just to
make sure that their numbers stay the same, but probiotics generally help the immune
system.
A lot of research has been conducted on probiotics ever
since it has been discovered that they’re essential for
our health, and although much of it is inconclusive (when it comes to
the bacteria that is ingested through supplements),
we do know that some species will help not only in the affections of the
digestive system but also in seemingly unrelated health problems.
Out of the more than 500 bacteria species that we naturally host in our bodies, some are very helpful and
work well when ingested from supplements, starting with Lactobacillus, especially the rhamnosus variety.
This strain is included in Perfect Biotics and can actually heal acute diarrhea, as demonstrated by tests performed on children. But
the other species of Lactobacillus are also very efficient in all types of intestinal disorders, with bulgaricus (also included) being able to help with
lactose intolerance. Also, this species of bacteria is the
only one that is completely harmless to the body. Generally speaking, all probiotics are, but they
could cause some unwanted effects in very sensitive people, and it seems
like this is never the case with L. bulgaricus.
Another strain of Lactobacillus included in this product is casei, which is commonly found in yogurt and
helps in protecting the body against harmful bacteria and will prevent affections like irritable
bowel syndrome and constipation. And L. salivarium has
similar effects, but also the added benefit of promoting dental health.
This one probiotic seems like it would help even the most healthy individuals,
and L. paracasei might have similar benefits. Studies performed on rats have
proven this strain to be effective against a bacterial species that promotes caries,
and it might just be effective for humans also.
And brevis, the last Lactobacillus strain included in this supplement, shows signs that might be effective in preventing
cancer and minimizing its damage.
The Bifidobacterium strains included in Perfect Biotic are very
useful also, with the first one on our list (lactis) being beneficial not
only in digestion and in the prevention and treatment of diarrhea,
but actually in the prevention of salmonella.
B. brevis on the other hand, the next strain, is generally only helpful for intestinal health but it amounts drop with age, and it’s a great addition to this supplement as
even individuals with no health issues will need it and benefit from ingesting it.
Then we have B. bifidum, which is the most common probiotic found in the human body but
at the same time very easy to kill through antibiotics.
It helps in preventing E. coli infections, and it should always be supplemented when using antibiotics.
B. longum is also common but it seems to have unusually beneficial properties,
as studies show that it might lower cholesterol
levels and even fight cancer.
And the last strain, B. infantis, is commonly found in breastfed
babies and also has very powerful effects. It can prevent salmonella
and E. coli infections, but it might also help in depression.
Is Perfect Biotics Safe?
Given that the product only contains probiotics, the only side effects that might be caused by using it are the usual intestinal issues associated with this type of bacteria.
Some people experience bloating, nausea, upset stomach, and other disorders for a few days after beginning the treatment,
but the symptoms clear out once the body adjusts.
But probiotics can also trigger allergic reactions, and all supplements of this type should be used
with a doctor’s approval. Each person has individual needs when it comes to probiotics, and just
because a product looks promising it doesn’t mean that it
will work well or that it’s fit for everybody.
Because Perfect Biotics doesn’t include other substances but
probiotics it’s also fit for children. But in this case, a doctor’s approval is mandatory, even if probiotics have been proven to work best for young patients.
It should be kept in mind that although good bacteria will
mostly bring positive changes, it does have the potential of becoming
dangerous in very sensitive or sick individuals.
Like all microorganisms, it could spread and act where it’s not supposed to, so potential users with
serious health issues need to make sure that the product is not dangerous for them before starting the treatment.
Perfect Biotics Benefits?
It looks like this product can only help, as it’s clearly able to improve digestion, boost the
immune system, decrease lactose intolerance and prevent dental issues along with many other benefits.
And because it contains such high amount of probiotics, it will
most likely act faster than many other similar supplements,
and help even in very problematic digestive disorders.
It will also stay fresh at room temperature, so this particular probiotic doesn’t need special care and
can be used whenever you might need it. But one serious
advantage that Perfect Biotics has over other products
is the high CFU count in a single capsule.
All 30 billion organisms will be ingested at one time, and this is recommended to be done only once a day, before breakfast.
Users will only have to remember it in the morning, so it doesn’t involve much hassle.
Why Choose Perfect Biotics?
This product looks very promising, and so does the company behind it.
As far as we know, Perfect Biotics is manufactured in good conditions and contains a high enough
number of strains and individual organisms to be very
effective. Also, the bacteria is alive at the time of the ingestion and packed in dark amber glass bottles that guarantee it’s protection from light.
And judging by the general opinion, customers seem to like all
products manufactured by the company.
Probiotic America looks to be very new but already has
happy customers, and it’s Twitter account (the only social platform that they’re active on) seems to prove it.
The account was created in June but already has over 900 followers, so it’s safe to assume that the products don’t commonly generate complaints.
And the way the products are marketed also helps this
company’s image, as it seems like they become available one at
a time, with lots of research between releases.
Perfect Biotics was the first and gave the impression that the company might not be legitimate (as many scammers focus on only one product), but soon it
became obvious that they’re planning on developing an entire line of supplements.
Meanwhile, another supplement based on probiotics was released,
and 5 more blends have been announced.
Actually, one pleasant surprise hidden in the «terms and conditions» section of the Probiotic America website is a disclaimer which states that
the products are constantly modified and improved, and different batches of the same supplement might have different properties.
This is a good sign for the company standing behind the products and constantly trying to make them more effective,
so it seems like they’re off to a good start. They also managed to avoid all the issues commonly associated with companies that sell their product on the internet, as they
disclose all the necessary information about the supplements,
are easy to contact and don’t hide important information in the user agreement.
They do seem to have an auto-shipping program, but it might not have anything in common with the practice that internet shoppers
hate the most, as we’ll see next.
Where Can I Buy Perfect Biotics?
You can buy Perfect Biotics through the official Probiotic America website, at the price of
$39.95 for a bottle containing one month’s supply.
Two discount packages are also available, with the one containing 3 bottles being sold for $101.87, and the
other, which includes six, being priced at $189.36,
with the latter reducing the individual price to a little over $30.
Shipping and handling for $4.95, but only when ordering one bottle.
Larger orders come with free delivery, but at this time, the company only ships
to the US.
Judging by some of the information in the user agreement it seems like things are going to change at one point, but one feature that
should stay the same is the 90-day money back guarantee
that applies to all products.
Given that Perfect Biotics’s effects should start being noticed
in around one month, it seems like this period is enough
for customers to evaluate the product.
And then there’s the auto-ship program. There is no sign for
it on the order form and we weren’t expecting to find anything
of the kind in the user agreement, but it seems like it does exist, and it
functions in a manner that makes it very different from the
usual money making scheme. This program is only available for customers located in the US, which shouldn’t be
necessary to mention given that the company only ships in this area, but it’s proof that Probiotic America is planning on expanding
their business somewhere in the future. And the
auto-ship program doesn’t actually function yet either (we
believe, as nothing in mentioned on the order form
and legally it should if this was the case), but when it will finally be available it will be optional
and allow customers to choose the exact schedule of the deliveries.
They will take place once every 30, 45, 60, 90 or
120 days, and the website also mentions that each delivery
will be notified to the customer after processing. The clients will be able to change the
settings of the program by logging into their accounts, and cancellation will be accessible at any time.
It really is made to seem like this system works to the
advantage of the customer, as it should given that this was it’s initial
purpose before being used by scammers.
In the end, Perfect Biotics looks to be as good as it gets
when it comes to supplements marketed through the internet,
and even with the auto-ship program, it seems like the company has the best intentions.
Hopefully, customer reviews will surface once the line of products is expanded, and we’re
expecting to hear about positive experiences. This is a paid,
third-party advertorial. The author receives compensation from the manufacturer of this product.
Hey I know this is off topic but I was wondering if you knew of any widgets I could
add to my blog that automatically tweet my newest twitter updates.
I’ve been looking for a plug-in like this for quite some time and was hoping maybe you would have some experience with something
like this. Please let me know if you run into anything.
I truly enjoy reading your blog and I look forward to your new updates.
This piece of writing will assist the internet visitors for setting up new
weblog or even a weblog from start to end.
http://wudikaoba.com/bbs/home.php?mod=space&uid=177363&do=profile&from=space
Good day! This is my first visit tto your blog! We are a team of volunteers
and starting a new initiative in a community in the same niche.
Youur blog provided us benneficial information to work on.
You have done a outstanding job!